
Health & Medicine
Better cancer treatments from better data analysis

The way we dose chemotherapy is crude. Cancer patients can end up with bad reactions that put them off continuing treatment. A new AI tool aims to change that
Published 13 June 2025
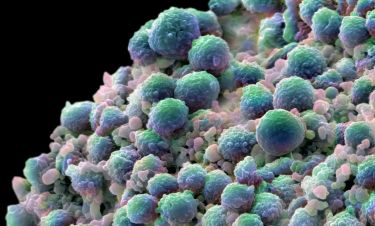
Chemotherapy is a vital treatment for people with all forms of cancer. It’s a process that uses drugs designed to kill, damage or slow the spread of cancer cells, preventing them from growing and dividing.
But the way we dose chemotherapy is still very crude. Around 60 per cent of patients are incorrectly dosed – either over or under. This inadvertently incorrect dosing can lead to distressing and difficult reactions that mean some people stop their cancer treatment too soon.

Our new AI algorithm aims to get chemotherapy dosing exactly right for colorectal cancer patients to improve their chances of living a full and happy life after cancer.
Colorectal cancer (CRC) is the second most common cause of cancer-related death in Australia. Internationally, more than 1.9 million new cases are diagnosed each year.
Around 50 per cent of these patients need chemotherapy treatment, which improves the overall survival rate by more than 30 per cent.
The current gold standard for chemotherapy dosing is based on a person’s body surface area (BSA), which comes from their weight and height (this is called the Mosteller Formula).
But this dosing calculation is highly inaccurate.

Health & Medicine
Better cancer treatments from better data analysis
The BSA doesn’t necessarily correlate to a patient’s body ‘make up’ – and it’s our body’s composition that determines chemotherapy dosing in several ways, including how effective active chemotherapy is metabolised and also how much toxic chemotherapy is stored within the body
This can mean that more than 60 per cent of all chemotherapy patients are inadvertently overdosed.
Too much chemotherapy can lead to significant side effects (known as toxicities). For example, neuropathies that affect sensation in a patient’s hands and feet; immunosuppression; cardiac and respiratory issues including heart attacks and chest infections; and gastrointestinal side effects like nausea and diarrhoea.
This is because two patients with the same BSA will have the same chemotherapy dose but may have completely different body compositions.
Let’s look at the bodies of a Sumo wrestler and a body builder. While their BSA might be similar, our Sumo wrestler has relatively more fat in their body, while the body builder has greater muscle.
But both would get the same doses of chemotherapy. However, because of their completely different body composition, this means they will develop different degrees of toxicity.
And the results of severe toxicities are serious.
It can mean someone stops chemotherapy early (at least 20 per cent of patients do), as well as more hospitalisations resulting in poorer quality of life, greater health economic impact and significant incidence of cancer treatment failure.
In fact, in five per cent of patients, this severe toxicity can result in death.
It’s these risks and reactions that can mean a person stops their treatment early, reducing their chances of going on to live cancer free.
Health & Medicine
The blood test tracking down microscopic cancer DNA
I work with people diagnosed with colorectal cancer every day. I’ve seen the severe changes to a patient’s health that the wrong dose of chemotherapy can cause.
And, for some patients, it can mean they decide that surgery is too much for them, resulting in a missed opportunity for a potential cure for their cancer.
Our team – a collaboration made up of Victorian hospitals, consumer groups, academic clinicians and scientists from the University of Melbourne and WEHI, as well as industry partners like Lenia Health – have developed PredicTx.
PredicTx is an AI algorithm that uses CT scans and the specific features of a person to accurately dose chemotherapy in colorectal cancer patients.
The aim is to ensure that most patients get the right chemotherapy dose and continue to get adequate and complete chemotherapy treatment.

And we have bold ambitions for what PredicTx could do.
Firstly, we want change in health practice.
We still rely on an archaic method of chemotherapy dosing based on BSA, which is highly inaccurate. Our tool aims to provide an AI-driven patient-tailored dosing solution.
We also want to increase access to chemotherapy treatment for all patients.
Ideally, PredicTx would mean that smaller and rural oncology providers could treat their patients with chemotherapy closer to home by reducing high-level hospital treatment when patients do experience complex toxicities due to incorrect dosing.

Health & Medicine
Who needs a colonoscopy most?
There are also priority groups – including older patients and patients who are culturally and linguistically diverse – who can be at higher risk of overdosing because of different body composition.
But overall, we want PredicTx to contribute to increased cancer cure rates through the successful completion of chemotherapy.
It’s amazing what we can achieve through collaboration.
Bringing consumers together with health institutions, universities and industry has brought PredicTx to life.
And while its focus is people with colorectal cancer right now – by getting chemotherapy doses right, it could bring us a step closer to making sure people with any form of cancer get the right amount of treatment at the right time. And keep getting that treatment.