Health & Medicine
Immunity to COVID-19: Lessons from malaria

New research is finding ways to beat dangerous superbugs with ‘resistance resistant’ antibiotics, and it could help in our fight against COVID-19 complications
Published 2 June 2020
Bacteria are a formidable foe when it comes to the war against illness.
As they evolve, bacteria develop strategies that undermine antibiotics and morph into ‘superbugs’ that can resist most available treatments and cause potentially lethal infections.
Combatting this problem is difficult, but University of Melbourne researchers are having some success in the fight against particularly virulent strains.
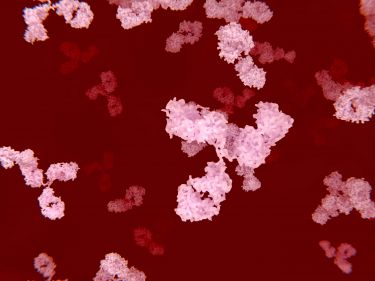
They have shown that a newly discovered ‘resistance resistant’ antibiotic could be effective in treating bacterial lung conditions such as tuberculosis and those commonly associated with COVID-19.
Their work with a recently discovered natural antibiotic, teixobactin, could pave the way for a new generation of treatments for particularly stubborn superbugs.
Health & Medicine
Immunity to COVID-19: Lessons from malaria
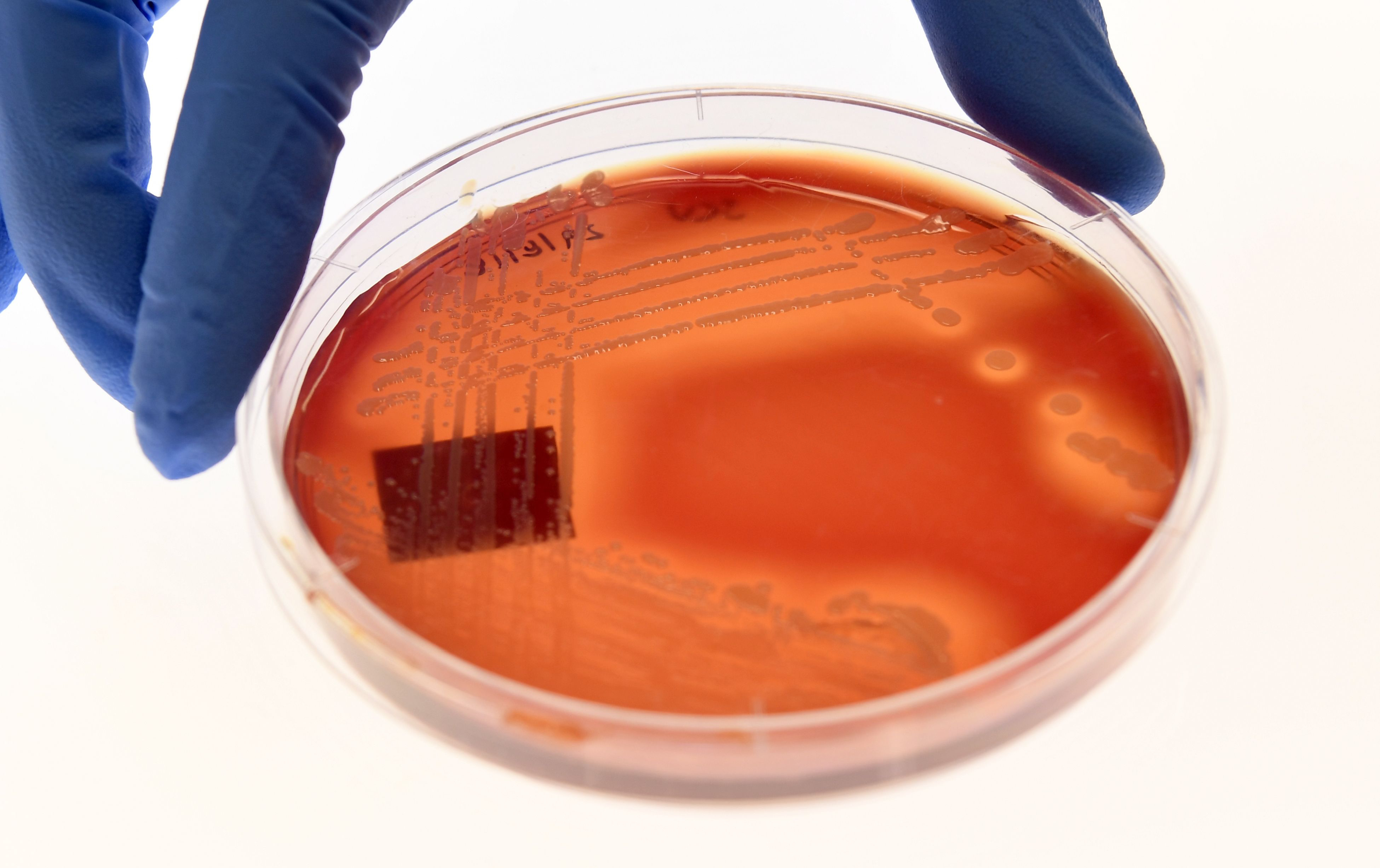
Teixobactin was discovered in 2015 by a team led by Professor Kim Lewis at Northeastern University in Boston in 2015. His company is now developing it as a human therapeutic. The new University of Melbourne research, published in mSystems journal, is the first to explain how teixobactin works in relation to the superbug Staphylococcus aureus – a bug you may have seen in headlines as MRSA.
Research Fellow in anti-infectives Dr Maytham Hussein and Associate Professor Tony Velkov’s team synthesised an aspect of teixobactin to produce a compound that showed excellent effectiveness against the virulent bacteria methicillin-resistant MRSA.
MRSA is among the bacteria responsible for several difficult-to-treat infections in humans, particularly post-viral secondary bacterial infections such as COVID-19 chest infections and influenza.

Dr Hussein explains that there is no way to stop bacteria like MSRA from developing resistance to antibiotics as it is part of its evolution. This makes combatting it extremely challenging.
“The rise of multi drug-resistant bacteria has become inevitable,” he says. “These bacteria cause many deadly infections, particularly in immunocompromised patients such as diabetic patients or those with cancers, or even elderly people with post-flu secondary bacterial infections.”
The problem is global, with the US Centers for Disease Control and Prevention (CDC) estimating that more than 80,000 aggressive MRSA infections and 11,000 related deaths occur in the US each year. It’s a similar situation in Australia, where MRSA remains a significant problem.
Health & Medicine
Understanding the response of our immune system’s powerful army
Antibiotic overuse is also an issue, and it can take 10 to 15 years to develop a new treatment, with a 95 per cent failure rate and huge development costs.
Dr Hussein is an infectious diseases specialist and part of a team internationally recognised in this constantly evolving field. A clinical pharmacist, he has worked in hospitals and seen antimicrobial resistance first-hand.
“There is no way to stop bacteria from developing antibiotics resistance as it’s part of their evolution,” he says. “Bacteria are smart creatures and they always develop strategies to undermine antibiotics.
“The superbugs are often resistant to almost all currently available antibiotics and cause infections with high mortality rates.”

Epidemiology models showed that simple infections could be more deadly than cancer, so Dr Hussein joined the “battle against bacteria” with experienced specialist Associate Professor Tony Velkov.
The University of Melbourne team is the first to find that teixobactin significantly suppressed mechanisms involved in resistance to vancomycin-based antibiotics. This could lead to new lung infection treatments.
Associate Professor Velkov says teixobactin was identified from soil bacterium Eleftheria terrae.

Health & Medicine
The COVID-19 treatment trials that ‘learn as they go’
“Our published data will greatly facilitate the pre-clinical development of teixobactin,” he says. “It holds much promise as a ‘resistant to resistance’ antibiotic for the highly resistant Gram-positive pathogens such as MRSA.
“These novel results will open doors to develop novel antibacterial drugs for the treatment of multi-drug resistant Gram-positive infections which are caused by certain types of bacteria.”
Working with teixobactin was time-consuming and exacting.
The team completed a global untargeted study, mined for thousands of metabolites and reconstructed complex pathways to understand the compound-killing mechanism.
They then exposed the superbug bacteria to the new analogue, or equivalent, of teixobactin.

“Bacteria often develop resistance towards antibiotics within 48 hours after exposure,” Dr Hussein says. “The bacteria failed to develop resistance towards this compound over 48 hours.
“We used a cutting-edge tool, namely metabolomics, which is a quite complex and sensitive platform. The accuracy, optimisation process and preparations are vital to get it done perfectly.
“We spent two to three months preparing, one month doing practical work and six months analysing data.”

Health & Medicine
How to take care of yourself if you have COVID-19
The rise of multiple drug resistant bacteria is a difficult war to win. The superbugs are numerous and potentially lethal, particularly for immunocompromised patients such as those with diabetes and cancer or elderly people with post flu secondary bacterial infections.
For this reason, Dr Hussein’s team is also using FDA-approved nonantibiotics and currently available antibiotics to fight them on several fronts. They have so far come up with at least six combinations.
“The FDA-approved compounds have already passed all safety measures with a known toxicity profile, so we basically save time and cost,” Dr Hussein says.
“Drug development is a very complex process, especially when developing new antibiotic classes that fit the criteria of being highly active, having acceptable pharmacokinetic properties, and being reasonably safe.”
Banner: Getty Images