
Politics & Society
How COVID-19 is hitting some democracies harder than others

How did one of the world’s most inequitable health care systems cope with COVID-19? The short answer is that it provides the starkest of warnings
Published 14 August 2020
You’ll notice the title of this article speaks in past tense.
When this article was imagined, we all hoped for a rapid and effective COVID-19 response justifying that ‘past tense’ frame.

For the United States, that has not occurred. It is now host to more documented COVID-19 cases and deaths than any other country.
With four per cent of the world’s population, the US accounts for approximately 25 per cent of all cases and 20 per cent of all deaths – more than 160,000 at time of writing.
Yes, it’s a large country, but that is 500 deaths per million population, compared to Australia’s twelve per million.

Politics & Society
How COVID-19 is hitting some democracies harder than others
As I pen this, the state of Victoria is amid its second wave, recording more than 700 cases in one day at the end of July. On the same day, the US recorded 68,543 new cases and 1,323 deaths.
I write this from my temporary base in the Washington, DC area.
I have experienced firsthand, and since the outset of the pandemic, how deficiencies in the organisation of the US social, political and healthcare systems have become more vivid and their consequences intensified.
Given its status as a world superpower, and its stratospheric per capita health care spend – it is a truly alarming state of affairs.
Entire books will be written on this woeful epoch in US history, but I want to focus on some key observations of the failed US COVID-19 response, and their lessons.

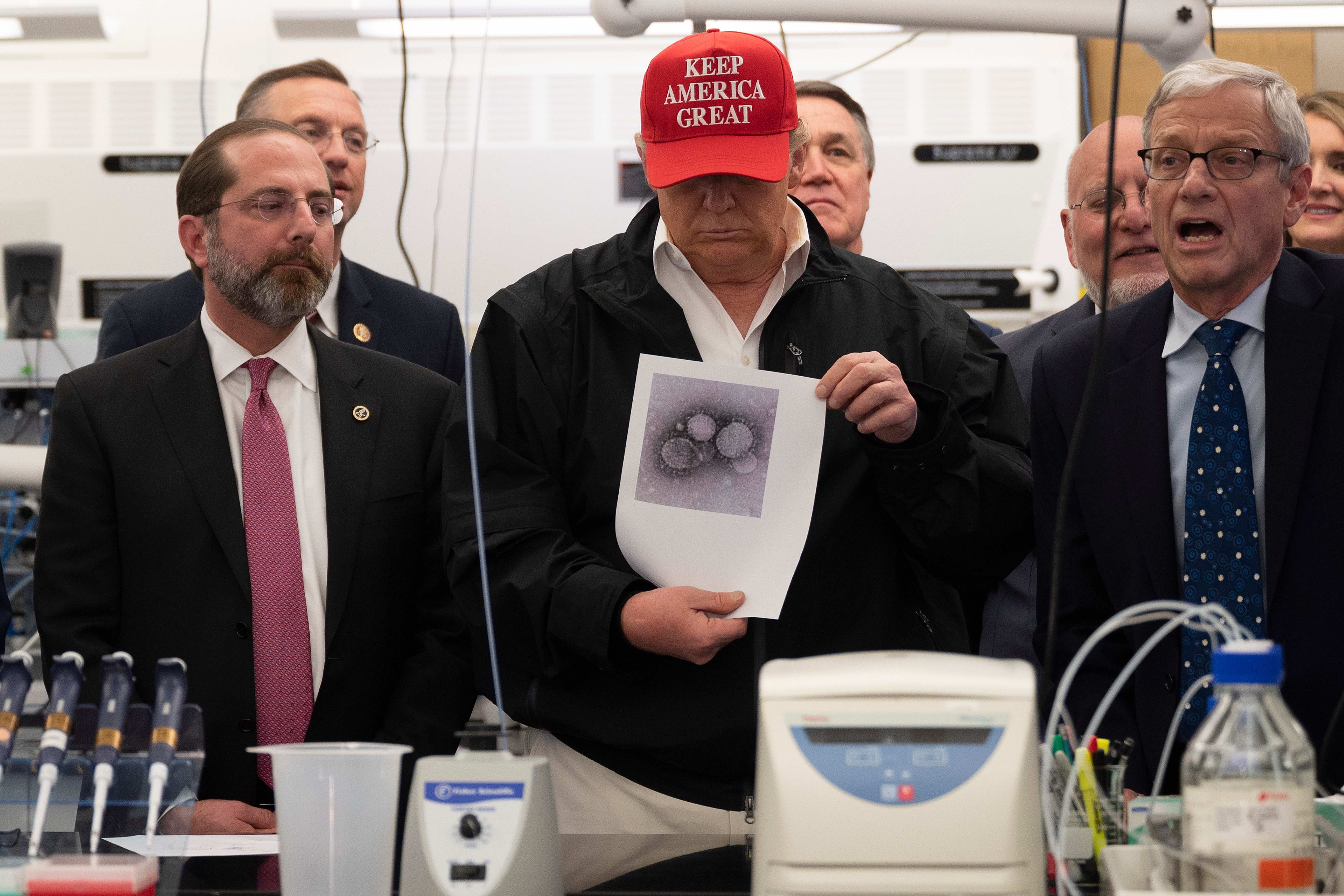
It would be unfair to blame President Trump and his administration for the systemic failures in the US social and health care systems. But, his pre-COVID-19 dismantling of the preparedness system, disregard for scientists and hyper-partisanship have clearly worsened the US response.
I agree with the political commentator David Frum who wrote: “That the pandemic occurred is not [President] Trump’s fault. The utter unpreparedness of the United States for a pandemic is Trump’s fault.”

Politics & Society
10 reasons why COVID-19 favours a Trump election victory
President Obama left the Trump administration with a pandemic-ready infrastructure, motivated by previous novel coronavirus and Ebola outbreaks and an appreciation of their ever-present threat.
Then, Trump took critical steps prior to COVID-19 that weakened its preparedness to the point of catastrophe.
Here are just a few.
The Trump administration dismantled the (Obama instituted) White House team in charge of pandemic response, dismissing its leadership and staff in early 2018.
This team had also laid out a detailed dossier for a pandemic response plan. Trump ignored it.
Further, since coming to office the Trump administration has cut funding to key agencies including the Centers for Disease Control and Prevention (CDC).
These cuts directly impacted domestic projects and international collaborations (including with China) on pandemic preparedness.
Even into February as the severity of the pandemic was realised worldwide, President Trump was downplaying the threat, openly stating it was like the common flu.

Politics & Society
Fake news in the age of COVID-19
He called growing concerns about COVID-19 a “hoax” a had a “hunch” that expert assessments of the potential toll were wrong.
As cases and deaths, particularly in New York began to rise steeply, the real evidence of unpreparedness became apparent.
Critically, at no point through the pandemic has the US had in place a sincere strategy of public health 101: test, trace, isolate.
Trump has repeatedly claimed that “anyone who wants a test can get a test” but this has been a complete farce. Shortages of testing supplies and poor coordination have hamstrung containment strategies.
Even though testing has increased, it has not kept up with demand and the time to receive results as of July ranged from one to 14 days, averaging seven days. This is simply inadequate to manage spread via active but undiagnosed cases.

And that is just the beginning of the current troubles.
The limited availability of masks, personal protective equipment (PPE) and ventilators not only revealed significant cracks in US preparedness but put on full display the caustic political divisions that is a modern feature of US politics and society.

Business & Economics
The COVID-19 responsibility we all own
Despite the first cases being recorded in Washington state, its deadly potential was initially felt most in the blue (Democratic) state of New York. Trump used this to avenge old scores and fuel competition between red (Republican) versus blue (Democratic) states.
When the New York health care system buckled as a result of its fragmented structure (another failing) and enormous caseload, the state’s Democratic Governor called for urgent assistance, such as supplies from the national stockpile.
In response Trump tweeted Governor Cuomo “should spend more time ‘doing’ and less time ‘complaining’”.
The fierce competition between states for limited mask and PPE supplies led to price gouging by suppliers.
Governor Cuomo should spend more time “doing” and less time “complaining”. Get out there and get the job done. Stop talking! We built you thousands of hospital beds that you didn’t need or use, gave large numbers of Ventilators that you should have had, and helped you with....
— Donald J. Trump (@realDonaldTrump) April 17, 2020
Frustration led governors to place clandestine international orders. Illinois and Maryland, for example, received plane loads of supplies under the cloak of darkness and protected by state police “out of fear the Trump administration would seize the cargo for the federal stockpile” – as occurred in Massachusetts.
There has also been tension across the country regarding stay-at-home orders, school closures, re-opening, data transparency and sharing – the list goes on.
Wearing a mask now represents political leanings and, concerningly, Trump has recently ordered COVID-related hospital data bypass the CDC and be fed directly to the White House, raising concerns about transparency.

Health & Medicine
How to take care of yourself if you have COVID-19
Despite Trump threatening his absolute authority, in fact much responsibility rests with state governors. And yet, counties (equivalent of local councils) in turn have enacted policies independent of and often contradicting state policies.
This could be sensible in reflecting local conditions as the rolling wave moves on. However, it has confused any singular messaging and exemplified the red/blue divide.
The southern (primarily red) states that were late to institute control measures and early to re-open are now the epicentre of this rolling wave.
Among countries in the Organisation for Economic Co-operation and Development (OECD), the level of structural inequality in the US is extreme and the collision of three problems (uncontrolled pandemic, recession, uninsured people) is disproportionately impacting the most vulnerable.

Pre-pandemic, approximately 32 million Americans (around 10 per cent of population) lacked any health insurance. A further 150 million (50 per cent of the population) held employer-sponsored health insurance.
Up until mid-June, 33 million Americans had filed for unemployment as a direct result of the pandemic, pushing the unemployment rate well into teen figures.
This number is rising weekly and millions of those have, or will, lose their employer-sponsored health insurance at a time they may need it most.

Politics & Society
Discrimination in a pandemic
The US has the unenviable first place position for the highest health care costs in the OECD (often cited as the leading cause of bankruptcy) and the worst health outcomes among similar countries.
COVID-19 has placed millions more Americans further away from accessing needed health care. The country was already experiencing a decline in life expectancy and the fear now is that this will be exacerbated further.
There is a political rallying cry used ad infinitum in the US that the country represents a shining light on the hill, a “beacon of hope” for the world.
We must admit the US population size and current political climate make its pandemic response more complex than countries like Australia. But that doesn’t mean we can be apathetic.

The US, through COVID-19, offers the starkest of warnings that underlying gross structural inequality, public health system underinvestment and unpreparedness and compounded socio-political tensions have met in a dizzying, tragic outcome for the richest country in the world.
All Americans have suffered but their most vulnerable have, and will continue to, suffer disproportionately more.
It is a shining light for what we must avoid, what we must stand up for and protect against.
Professor Elshaug’s spouse is Chief Medical Officer for a US ventilator manufacturer that is responding to the pandemic.
A version of this article was co-published with The Conversation.
Banner: Getty Images