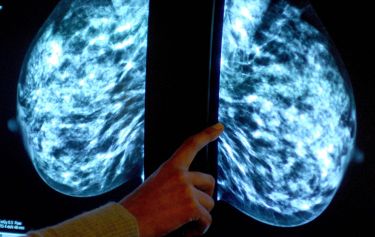
Health & Medicine
Filling in the genetic blanks of breast cancer predisposition

Associate Professor Clara Gaff is the Executive Director of the Melbourne Genomics Health Alliance – a collaboration dedicated to bringing genomics, the testing of all genes, into healthcare.
Published 9 April 2019
My family is very scientific. My mother was a science teacher and my father – although retired, is still active academically – a research scientist in botany or plant physiology to be exact. I grew up immersed in science. When I was little, my father took us with him on a year’s sabbatical in South Africa.
We would be playing while he collected plants that could survive drought. Although I was only four years old, I have very clear memories of that year. The landscape was so radically different to suburban Melbourne that it created a deep impression. I mostly remember outdoor things – guinea fowl running around outside, avenues of jacaranda, a hippopotamus at Kruger national park.

Back in Melbourne, mum would take us down to the creek to get pond water, then put it under the microscope at home and show us the tiny organisms swimming around in it. We’d look at the cells in drops of blood, or she’d buy lambs brains for a meal and show us the different parts when she was preparing them.
There was always a sense that science is happening everywhere. I think it instilled a curiosity in me, or maybe I found it interesting because I was curious? Wanting to continually learn was part of what made science attractive as a career. Also, studying science at school was kind of a requirement; my parents believed if we did science and maths, we could do anything after that.
Health & Medicine
Filling in the genetic blanks of breast cancer predisposition
Genetics just made sense to me. Mum and dad had always talked about recessive genes, dominant genes, x-linked inheritance, things like that. I studied science and majored in genetics at the University of Melbourne. I look back now and think: “We know so much more than we did then.”
At the end of my degree I was interested in becoming a genetic counsellor, but was told you had to be a doctor or a nurse. So, I did a PhD at the Walter and Eliza Hall Institute, and that was a pivotal point in my career. My peers from that time are people I have continued to work with over the years, including WEHI Director Professor Doug Hilton.
A genetic counsellor works with families who have (or are concerned they may have) a genetic condition. They guide and support people, and seek relevant information about personal or family medical history. A genetic counsellor may discuss the possibility of testing, and assist families to adjust to the diagnosis of a genetic condition in themselves or their child. Fundamental to genetic counselling is the notion of respecting individual decisions – it’s about people making decisions that fit their values and belief systems.

I was the first genetic counsellor involved in a pilot hereditary colorectal cancer program at the Royal Melbourne Hospital – a program that led to the current Familial Cancer Centre. I did postgraduate studies in health services research and evaluation, in order to understand how to evaluate what we were doing. The need for evidence of what works really influenced the work I do now.

Health & Medicine
Big data puts genomic handbrake on cancer
The Melbourne Genomics Health Alliance came about when I was working on collaborations in personalised medicine, both at the Victorian Comprehensive Cancer Centre and the Walter and Eliza Hall Institute. Chief Executives from across the Parkville precinct (hospitals, research organisations and the University) were talking about how their organisations could work together in genomics.
Doug Hilton asked me to develop a vision for what that collaboration might yield in five years, and that was really the birth of the Melbourne Genomics idea. The seven founding Alliance member organisations each put $A250,000 on the table for the first year, to undertake a demonstration project.
Five years ago when we started, there were four of us at Melbourne Genomics – now we can count more than 500 people involved. The initial $A1.5 million investment has now grown to a total of $A39 million: $A26 million from the Victorian Government and the rest from the member organisations (the seven founders – The Royal Melbourne Hospital, The Royal Children’s Hospital, The University of Melbourne, Walter and Eliza Hall Institute, Murdoch Children’s Research Institute, CSIRO, and the Australian Genome Research Facility – along with Austin Health, Monash Health and Peter MacCallum Cancer Centre joining in 2015. The program has leveraged an estimated $A60 million in clinical and research funds for the Alliance’s 10 members.

When we started, there was no evidence for the value of genomics in clinical care, no clinical funding for genomic tests, anxiety from clinicians about what the impact would be on their work and laboratories doing largely what we call ‘panel’ tests – sequencing a set number of genes.
Now, laboratories are sequencing all genes at once – a test called ‘whole exome sequencing’. We have evidence that patients this testing will benefit clinically, as well as economically. For one condition, there were five times more diagnoses than usual at one quarter the cost – so we can show how this testing reduces waste in the healthcare system. The challenge now is how to ensure testing is used widely and wisely.

Health & Medicine
Wiping cancer from our hard drives
Over the five-year period to date, we’ve enabled 3,720 patients to receive genomic testing. The results of those tests benefit not only those patients, but can be used to guide policy decisions about funding. The Medical Services Advisory Committee recently recommended that whole exome analysis should be funded by Medicare for children with suspected genetic conditions and the data supporting that recommendation came from our work.
The work we have done in Victoria has been rolled out nationally. For example, rapid genomic testing. Instead of taking three to six months to get a test result, we can now get results in just a few days for babies in intensive care, so answers can be delivered in a time-frame that will make a difference. That work has had startling results – more than half of those babies have had a change in care.
In the early 1990s, less than a handful of genes were tested clinically and none were sequenced. I could never have imagined that now we would routinely do a single test where 20,000 genes can be sequenced – and more than 3,000 of those genes are known to cause disease – let alone that this could be done so quickly for critically unwell children.

I was recently awarded the Most Valuable Women in Leadership Award in the 2019 BioMelbourne Network Women in Leadership Awards. The award recognised my efforts in establishing and leading Melbourne Genomics and accelerating the translation of genomics from research into patient care.
I first thought, ‘this work is really making a difference’ when a father’s letter was read on ABC Radio Melbourne, on Raf Epstein’s Changing Tracks program, in late 2014. The father spoke very movingly of the difference genomic testing (funded through Melbourne Genomics) had made for him and his family. He vividly described the journey from thinking about his child’s funeral to his child receiving treatment and having a future. It was really life-changing for them.
My work constantly reminds me that when we talk about numbers and percentages, under each of those numbers are people, whose lives are being impacted in a positive way by genomic testing.
- As told to Michelle Henderson
Banner: Getty Images