Health & Medicine
Immunity to COVID-19: Lessons from malaria
In Australia, amid the COVID-19 pandemic, we take oxygen access in our hospitals for granted. But new research is working to ‘close the oxygen gap’ globally and potentially change the world
Published 29 September 2020
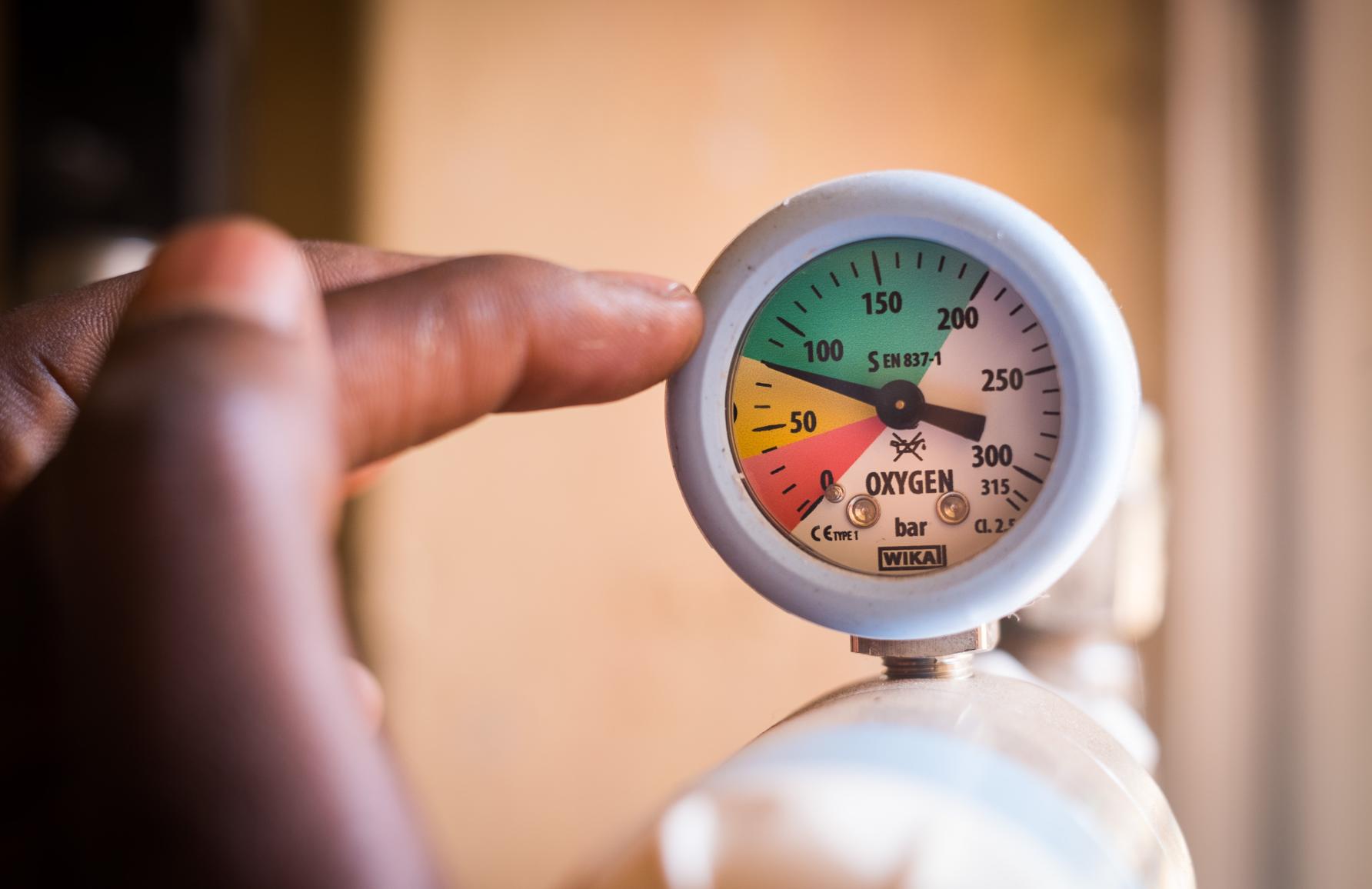
In recent months, emergency rooms and intensive care units around the world have been overwhelmed with COVID-19 patients – bringing into sharp relief how utterly reliant we are on oxygen and how much those of us in high-income countries take it for granted.
Several years ago, I was working in a small clinic in Sudan.

A small girl named Amina* was brought in, clearly very unwell with pneumonia. She was breathing fast and barely conscious. We gave her antibiotics, connected her to our sole oxygen concentrator and admitted her to the ward.
Amina kept getting sicker, but other unwell patients also needed oxygen, forcing us to choose who to prioritise.
Since then, I’ve learned that oxygen access is a universal challenge for hospitals in low and middle-income countries (LMIC) like Sudan.
Health & Medicine
Immunity to COVID-19: Lessons from malaria
In fact, we estimate that every year, around 15 million children like Amina are admitted to hospital with life-threatening low blood oxygen levels due to pneumonia and other conditions in which lack of oxygen is a major contributor to death.
Nearly all of those children, 90 per cent, come from low-income countries in the African and Asia-Pacific regions where better oxygen access could prevent over half a million child deaths annually.
Earlier this year, our study of 12 district hospitals in Nigeria showed that 80 per cent of children with severely low blood oxygen levels did not have access to oxygen therapy when they needed it.

Where oxygen equipment was available, it was often faulty, and many nurses were not equipped to measure blood oxygen levels – something that can be easily measured using a pulse oximeter.
Pulse oximetry is a quick, simple and non-invasive method of measuring blood oxygen levels, using a sensor to measure light absorption through body tissues to calculate the blood oxygen saturation.
But, in places like Nigeria, oximeters are rarely available outside the operating theatre. This means that most patients who need oxygen aren’t recognised – while scarce oxygen resources are wasted on patients who may not need it.

Health & Medicine
The breath of life
Introducing pulse oximetry as a routine part of assessment dramatically improves both the identification of who needs oxygen, and actual provision of oxygen patients.
Similar gaps in oxygen access are found in hospitals across sub-Saharan Africa and Asia-Pacific – particularly in small and medium-sized hospitals.
COVID-19 has brought a double-burden to many low and middle-income countries and threatens to further overwhelm hospital oxygen systems. Approximately 20 per cent of COVID-19 patients globally have required hospital admission for oxygen therapy – so closing the ‘oxygen gap’ must become a global priority.
Our new research, published in Global Health Science and Practice, outlines the practical ways hospitals can immediately strengthen their oxygen systems – to meet both COVID-19 needs, and build a better future.

Oxygen therapy is an essential medicine that has been around for over a century.
It’s a core component of effective hospital systems and a basic standard of care for pneumonia, surgery and many other health issues.
But many health facilities in LMICs lack reliable oxygen access – a deficiency that has been both highlighted, and exacerbated, by the COVID-19 pandemic.

Health & Medicine
The vaccine saving the lives of Pacific children
There are three major challenges to oxygen access:
1) low-quality, poorly functioning equipment, with inadequate access to maintenance and repair support
2) lack of clinical and technical education and protocols, including particular lack of awareness regarding pulse oximetry
3) deficiencies in local infrastructure and management systems, including unclear policy or financing guidance for oxygen-related investment
Our team of Melbourne-based paediatricians and researchers have been supporting hospitals and governments to build stronger oxygen systems in Africa and Asia-Pacific regions for more than two decades.

Our results, published with partners in Nigeria, Laos and Papua New Guinea, show that strengthening hospital oxygen systems can reduce a child’s risk of dying from pneumonia in hospital by 35 to 50 per cent.
As the COVID-19 pandemic has unfolded, we worked with country partners and UN agencies to support the inclusion of pulse oximetry and oxygen access in COVID-19 response efforts.

Business & Economics
Finding new ways to track COVID-19 exposure
A host of new technical guidance documents for oxygen are now available in the WHO COVID-19 Technical Guidance hub.
With the support of multiple donors, UNICEF has delivered almost 15,000 oxygen concentrators and around 15,000 pulse oximeters to 69 countries – with many other donors sourcing and delivering equipment directly.
This presents both opportunities and challenges for long-term oxygen access.
COVID-19 has meant the major focus has been on the treatment of adults in COVID-19 facilities – typically in large, urban hospitals.
But this could further disadvantage smaller, more rural hospitals – and children.

In fact, for most LMICs, the greatest long-term impact of COVID-19 will not be direct COVID-19 deaths – but the indirect impacts, with predictions of up to one million excess child deaths due to failure of basic health services.
So, maintaining key hospital services – like oxygen – is essential.
This is what has driven us to make all our protocols, user guides and practical manuals freely available in an online oxygen resources repository (now hosted by UNICEF) and joined with collaborators in Africa to share key lessons on how to rapidly improve hospital oxygen systems for COVID-19 and the long-term.

Business & Economics
The lessons from past pandemics
There are clearly bigger structural challenges that prevent an old, well-established, medical therapy being routinely available in LMIC hospitals.
Oxygen relies on equipment – but not just one piece of equipment – and the best combination of oxygen sources and delivery components depend on the context.
Private markets for oxygen have largely failed LMICs, particularly for smaller, rural hospitals (although there are some promising models being developed). Oxygen is not yet included in standard cost-effectiveness calculators like the Lives Saved Tool (we’re working on it).

However, there is increasing evidence for oxygen’s cost-effectiveness and growing awareness of what’s needed to take oxygen system improvement to scale.
Our team, and our international partners, have applied (and occasionally been supported) through grants from organisations like the Bill and Melinda Gates Foundation, Unitaid, and USAID to improve oxygen access.
But now we are looking to compete to take oxygen to scale.

Health & Medicine
Immunising kids against pneumonia
The US-based MacArthur Foundation’s 100&Change competition provides $US100 million to a single proposal that promises to make measurable and lasting change to a significant global problem.
We think oxygen access is that global problem.
Together with our US-based partner, Clinton Health Access Initiative (CHAI), we are now through to the final six. Our focus is on five countries — India, Nigeria, Ethiopia, Kenya and Uganda — which together account for an estimated one-third of global cases where lack of oxygen is a major contributor to death.
If we succeed (and we are up against some excellent proposals), the resulting improved oxygen systems will help save lives not only in this pandemic, but many more into the future.
*Not her real name
Banner: Supplied