
Health & Medicine
Why 2025 is a big year in women's health
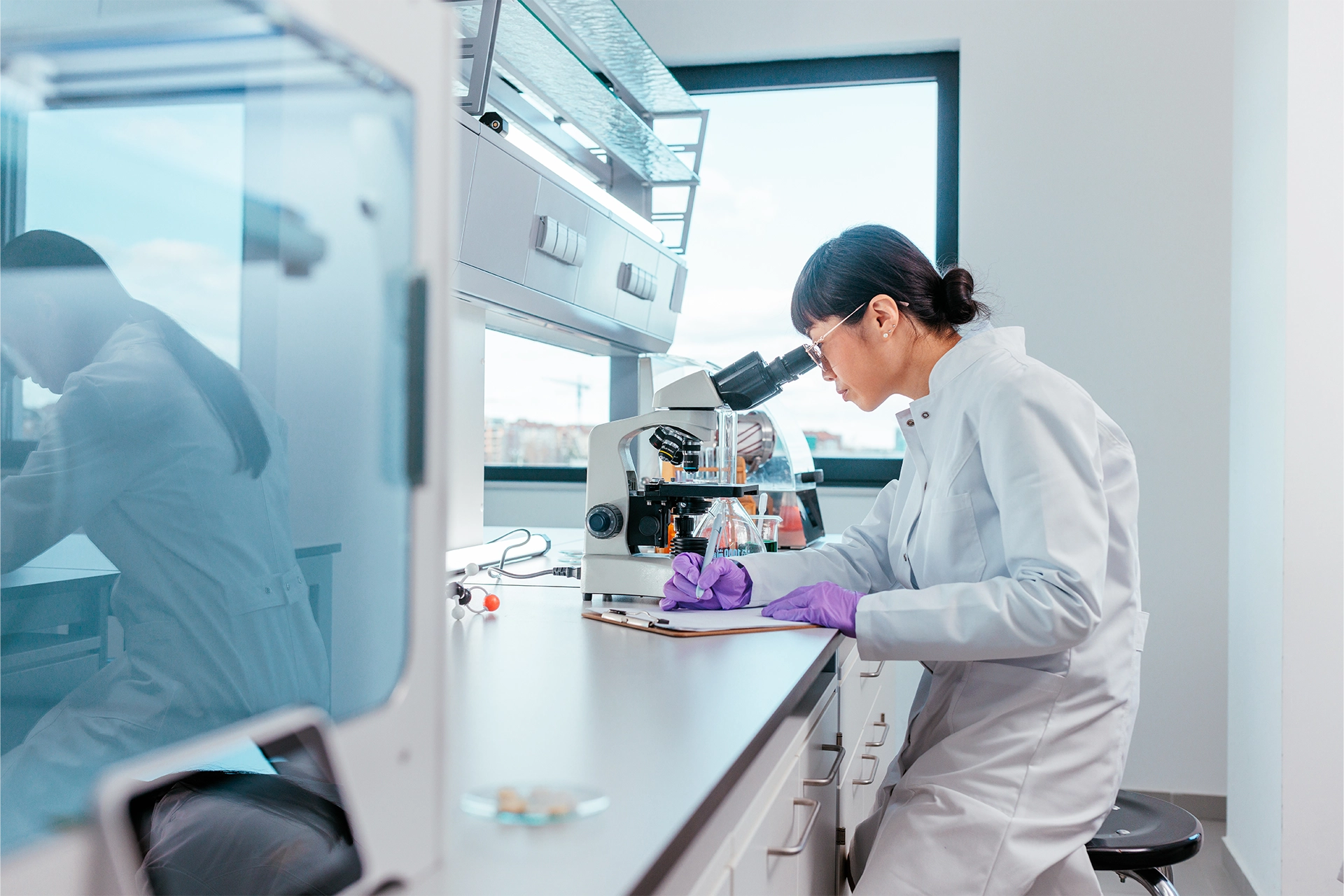
By listening to women’s voices and investing in targeted research, Australia is taking important steps towards creating a more equitable healthcare system
Published 7 March 2025
Women’s health is finally becoming a national priority. The Australian government’s recent commitment of $AU573.3 million to strengthen Medicare for women is the signal many of us had been waiting for.
As we celebrate International Women’s Day, it’s the perfect time to take a look back at how funding for women’s health has evolved over the decades – and why it matters so much.

Imagine visiting a doctor and not being taken seriously because your symptoms don’t match the ‘default’ picture of human health – a picture based on male bodies.
This issue, known as the ‘pain gap’, exposes how discrimination – whether from biological differences or gender stereotypes – undermines care for women.
Before the late 1980s, drug trials in the US (where most drugs are developed) routinely excluded women of childbearing age, so medical research has long used male bodies as the norm for diagnosis and treatment.
As a result, women often face misdiagnoses or delayed treatment.

Health & Medicine
Why 2025 is a big year in women's health
For example, heart attack symptoms in women are more likely to be overlooked.
And despite the significant hormonal changes brought about by menopause, research on this transition remains scarce and this just further widens the gap.
Australia’s journey toward better women’s health started in 1989 with the first National Women’s Health Policy, when the government introduced a comprehensive plan that went beyond reproductive health to include a broader range of women’s needs.
Breast and cervical cancer screening programs started soon after in 1991.

The next major milestone was the establishment of the Australian Longitudinal Study on Women’s Health, which has tracked the wellbeing of women over generations since 1996.
In 2007, Australia became the first country to rollout the human papillomavirus (HPV) vaccine and extended the program to include boys in 2013. The vaccine remains free today for people under 26, but costs increase insignificantly beyond this age.
By 2010, the country reaffirmed its commitment with the National Women’s Health Policy 2010, focusing on prevention, mental health, chronic disease management and healthy ageing.
A decade later, the government’s current National Women’s Health Strategy 2020–2030 recognises that women’s health isn’t just about childbirth or fertility, but about a full spectrum of challenges that women face at different stages of their lives – from period pain to menopause.

Health & Medicine
All young people should get the HPV vaccine – girls and boys
While these steps indicate a positive trend in both the recognition and treatment of women’s health conditions, the National Women’s Health Advisory Council’s #EndGenderBias survey tells us there’s still a way to go.
Conducted in 2023, the survey collected responses from over 2,570 women, 86 caregivers and nearly 500 experts.
It revealed that about two-thirds of women have experienced bias or discrimination in healthcare.
The most common issues women reported included being dismissed by their healthcare provider, having their symptoms labelled as “emotional,” and experiencing obstacles in accessing affordable, quality care.

Recent funding packages announced in 2022 and 2023 were dedicated to tackling a series of women’s health issues, including:
Over $AU58 million to improve care for endometriosis and pelvic pain, with funding going to GP clinics, primary care, clinical trials, digital platforms and awareness campaigns
$AU103.7 million worth of new investments in maternal, sexual and reproductive health, including updates to obstetrics and gynaecology services, universal genetic testing and improved support for rural maternity care
$AU23 million to support families who experience stillbirth or miscarriage
Over $AU142 million to expand services for victims of domestic and sexual violence, including trauma care and recovery centres
Additional investments for priority groups including Aboriginal and Torres Strait Islander women, migrant women and women with disabilities
Almost $AU25 million for better cancer screening and prevention services
More than $AU3 million to establish a National Women’s Health Advisory Council and continue the Australian Longitudinal Study on Women’s Health
Around $AU10.3 million to support women’s sports initiatives promoting leadership, safety, and employment for women and girls.

Health & Medicine
5 things you didn’t realise you need to know about perimenopause
In September 2024, the government also launched their $AU10 million campaign to boost cervical cancer screening, aiming to eliminate the disease by 2035.
The government’s most recent $AU573.3 million funding announcement in February 2025 builds on this progress, as well as promising investment in several new initiatives.
For the first time in over 30 years, new oral contraceptive pills will be listed on Australia's Pharmaceutical Benefits Scheme (PBS), making them more affordable for around 50,000 women annually.
Women will also have access to more birth control options, including being eligible for larger Medicare rebates for IUDs and other birth control implants, helping around about 300,000 women to save up to $AU400 each year.

Menopause is another focus, with new Medicare rebates promised for menopause health assessments, as well as new clinical guidelines, professional training and a national awareness campaign, benefitting roughly 150,000 women in total.
New menopausal hormone therapies will also be listed on the PBS.
For women living with endometriosis and pelvic pain, the government announced plans to open 11 new endometriosis clinics and boost staffing at existing clinics, making specialist support more widely available.
And as part of two new national trials, pharmacists can provide contraceptives and treatment for uncomplicated urinary tract infections – meaning around 250,000 concession cardholders will be able to access more convenient and affordable care without always needing to see their GP.
Sciences & Technology
Women living with chronic pain aren’t getting enough support at work
These initiatives mark significant progress, but challenges still remain.
Women’s health has long been shaped by outdated norms that prioritise male experiences, a bias that still influences diagnosis and treatment and affects women’s overall health, work and quality of life.
Women in rural areas and marginalised communities often face extra hurdles in accessing quality care.
While more funding is a huge achievement, we must also raise awareness across all sectors.
Health professionals need training on gender differences, and schools and workplaces need to adopt clear policies for issues like period pain and menopause symptoms that don't force women to conceal their struggles.

Looking ahead, these changes offer hope and a clear direction for the future of healthcare where all women can receive affordable, tailored care – and where their symptoms are correctly identified.
By listening to women’s voices, investing in research and implementing practical improvements, Australia is taking important steps toward a more equitable future.