Health & Medicine
Filling in the genetic blanks of breast cancer predisposition

Medications and supplements aimed at preventing cancer, called chemoprevention, can lower the risk of the disease, but patients need to be clearly informed of the side effects. Here’s how.
Published 28 April 2019
Every year, the ways that doctors can diagnose and treat cancer are becoming more sophisticated.
To date, prevention of cancer in primary care has focused on modifying behaviours associated with increased risk of cancer – primary prevention – or increasing participation in national cancer screening programs, known as secondary prevention.

But if you are someone at a higher risk of developing cancer, there are approaches that can prevent it forming in the first place, known as chemoprevention. Chemoprevention can include the use of medication to lower risks, delay development or recurrence of cancer, or even to try and prevent it altogether.
Now it’s entering general practice for specific groups of patients.
But all medications have potential side effects and the potential harms and benefits of cancer chemoprevention must be clearly explained to patients. And how these risks and side effects are explained to people is important.
Health & Medicine
Filling in the genetic blanks of breast cancer predisposition
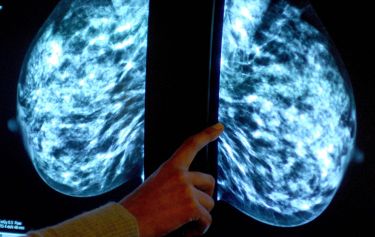
Researchers from the University of Melbourne Cancer in Primary Care Research Group have developed a new way of communicating this information using diagrams called ‘expected frequency trees’.
The team developed the diagrams to illustrate the effects of aspirin to reduce the risk of developing bowel cancer in people aged 50 to 70-years-old. They also used the expected frequency tree diagram to explain the use of drugs called selective oestrogen receptor modulators (SERMs) for women at increased risk of breast cancer.
The team explored the clinical implications of relatively new Australian guidelines on the prevention, early detection and management of bowel cancer which includes prescribing risk-reducing medication for bowel cancer.
The guidelines were released by the National Health and Medical Research Council in 2017, and were led by Cancer Council Australia with contributions from Professor Jon Emery of University of Melbourne.
Studies have found that taking aspirin for as little as two-and-a-half years can reduce the incidence of bowel cancer, with those people who are at increased risk of bowel cancer more likely to benefit than those at average risk of bowel cancer.
Overall, studies found benefits like reducing the risk of heart attacks and the reduction in bowel cancer, significantly outweighed potential harms from aspirin use, like gastrointestinal bleeding.

Health & Medicine
Targeting ovarian cancer
It’s estimated that for a person aged 50 years, taking aspirin for 10 years is 10 times more likely to prevent death than cause it, and this is five times more likely for someone aged 65 years.
For the study, Professor Jon Emery, Dr Jennifer Walker, Dr Jesse Minshall, Ms Kara-Lynne Cummings and Mr Peter Nguyen developed new risk communication methods, including the ‘expected frequency trees’, to show what would happen to 10,000 men and women in Australia aged 50–70 years if they took aspirin.
The diagrams – which have a trunk and branches – show likely outcomes over 10 years of taking aspirin for at least five years. These visual summaries aim to present the likelihood of specific outcomes to help patients make more informed decisions about treatment.

Peter Nguyen, PhD candidate in the Cancer in Primary Care group at the University of Melbourne, conducted a study with general practice patients to evaluate risk communication methods, including the expected frequency tree, for aspirin use as an Honours student last year. He noted the importance of involving patients in the treatment choice process.
“There is a shift towards encouraging shared decision making, showing patients the benefits and harms to inform whether they want to take medications for cancer prevention,” Mr Nguyen said.
“This research clearly shows that the benefits of taking aspirin for bowel cancer prevention still outweigh any potential harms in the cohort of 50–70-year-old patients, even over long periods of time.”
Health & Medicine
Our cancer preventing genes revealed
For breast cancer prevention, several randomised controlled trials have shown that drugs such as tamoxifen and raloxifene (so-called SERMs) significantly reduce the risk of breast cancer in women who have no personal history of the condition.
Analysis of data from nine prevention trials showed 38 per cent reduced incidence of breast cancer. Participants included women at increased risk of breast cancer as well as those at average risk, and both premenopausal and postmenopausal women. Australian guidelines recommend that women at increased risk of breast cancer, due to their family history, should consider the use of SERMs to prevent breast cancer.
The expected frequency trees aim to clearly display benefits and side-effects of taking three different SERMs for chemoprevention for breast cancer.
The trees show that the decision to take an SERM is potentially more complex than it is for aspirin. Women with a family history of breast cancer who are interested in exploring SERMs for chemoprevention may be better referred to a familial cancer clinic or specialist breast cancer service. The discussion about taking aspirin for bowel cancer prevention could sit well within primary care.
The guidelines for aspirin and SERMs reflect a new approach to cancer prevention in primary care.
The decision to prescribe these drugs involves careful discussion with a patient about the potential benefits and harms and consideration of underlying disease risks. The decision trees can be important and effective tools to guide and inform vital prevention discussions with patients.
Banner: Shutterstock