
Health & Medicine
Healthcare has a waste problem, but we can achieve net zero

The Healthcare Carbon Lab aims to reduce carbon emissions in our health sector by measuring carbon-emitting procedures and products, while still delivering quality care
Published 9 July 2024
Healthcare is one of Australia’s heaviest polluters, contributing around seven percent to our national carbon emissions. At the same time its one of our most essential sectors.
The enduring challenge we have is maintaining quality, while improving sustainability.
Consider this.
At the height of the COVID lockdowns in 2021, the carbon footprint of Australian healthcare amounted to 35.8 million tonnes of CO₂e (or carbon dioxide equivalent) emissions.
So you have an idea of that magnitude, we know that under normal circumstances, one person’s average carbon emissions for an entire year – that's all their energy use from heating and cooling, transport, gadgets, appliances and food – is about 15 tonnes.
This means that in Australia the carbon footprint of business-as-usual healthcare is equivalent to the entire population of Brisbane’s everyday usage – for a year.
We also know that around a third of clinical care is low value or even harmful care which includes things like excessive pathology and radiology testing, sometimes with false positives .
And with it comes wasteful use of equipment and energy in hospitals.
The electricity and gas that powers hospitals accounts for about 20 percent of emissions in the healthcare sector.
This contribution to the atmosphere is virtually permanent, lasting anywhere from 500 to several thousand years.

Health & Medicine
Healthcare has a waste problem, but we can achieve net zero
While we know the magnitude of healthcare’s emissions, we do not currently have detailed information about the emissions associated with specific medical consumables, devices or procedures.
Without this knowing this, we can’t effectively mitigate emissions.
The Healthcare Carbon Lab is a new collaboration that aims to gather data about emissions inherent in healthcare.
In a collaboration between the Faculty of Medicine, Dentistry and Health Sciences and Western Health, the lab uses a gold-standard approach to measure the carbon footprint of clinical areas, and then works to develop innovative solutions to decarbonise healthcare.
Just like human bodies, a hospital is an extremely complex system.
Patients enter a hospital to receive care from teams of highly trained healthcare professionals.
To do this properly requires the use of energy, equipment and drugs to diagnose and treat patients.
In acute care settings – like hospital emergency departments and intensive care units – lives are saved every day. People with severe or life-threatening illnesses may be put on life-support machines that maintain their bodily functions, helping them to recover.
People’s lives are on the line and all necessary resources are invested in their care and recovery.
These resources all come with a carbon footprint.
While the first step in reducing healthcare's carbon footprint is to avoid hospital, by providing access to quality and timely primary care and prevention in the community, that's not always possible.
1 / 4
Any of us may need hospital care one day, whether it’s to safely birth our baby, access treatment for acute COVID infection, for surgery, or other treatments for a debilitating or life-threatening condition or injury.
But high-value, sustainable care doesn't necessarily need to conflict.
In fact, it is achievable.
Individual healthcare specialists and their teams make hundreds of daily decisions; the gowns they wear, the equipment they order, the number of tests they request, how they administer medication and which gases they use for anaesthesia.
These decisions can create change across the healthcare system.
But how do healthcare specialists make more environmentally sustainable decisions in a complex, fast-paced environment while trying to save lives ?
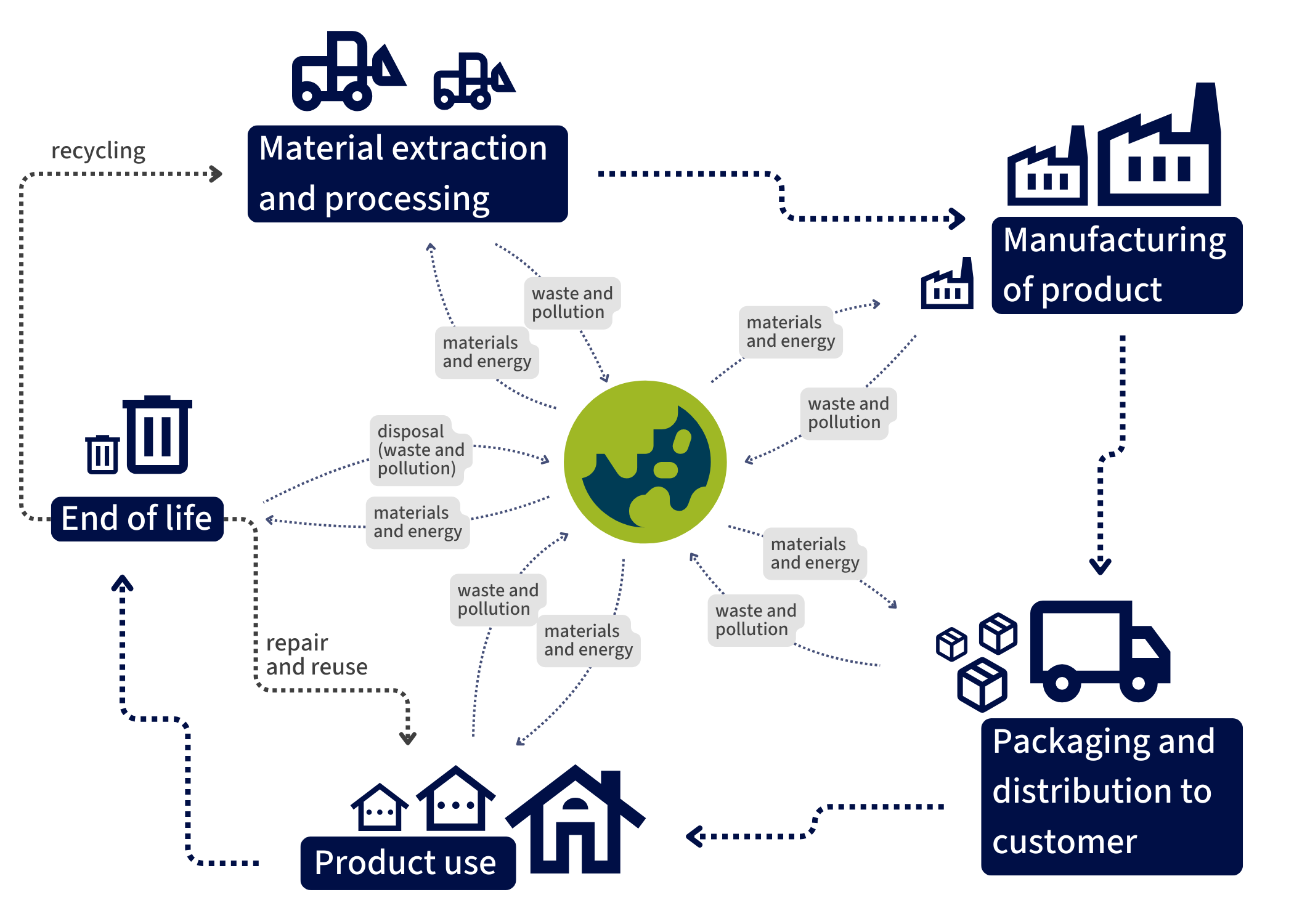
This is where a Life Cycle Assessment (LCA) can provide a systematic approach for strategic decisions.
An LCA makes it possible to calculate the environmental footprint for all healthcare equipment or ‘stuff used’ by tracking and calculating the energy used in its creation, use and disposal – from the ‘cradle to the grave’.
Even before it reaches the hospital, the lifecycle of stuff begins.
Firstly, there's the extraction of the material required to make the item, then its manufacture and processing.
Then there's its transport; its purchase and use in the hospital or healthcare setting and ultimately its disposal, or ‘grave’. The phases of an LCA are defined in the ISO (International Organization of Standards).

Health & Medicine
The economics of good health
As part of an LCA, to understand the energy and equipment used across the healthcare system, we need to measure or count it.
This is called a Life Cycle Inventory (LCI) and includes data on the energy used for lighting and managing room temperature, as well as equipment in processes like an MRI or ultrasound.
It also includes patient ‘consumables’ – like washing and drying bed linen or running diagnostic pathology tests.
In surgery, it includes anaesthesia drugs and the sterilisation of surgical equipment.
For staff, it's personal protective clothing (PPE) to keep both themselves and patients safe from the transmission of infectious agents, including masks, gowns and gloves.
So, as an example, a LCA of patients in an intensive care unit (ICU) in Melbourne with septic shock told us the majority of that carbon footprint resulted from the gas needed to heat the ICU, with lesser emissions coming from LCI items such as plastic equipment, PPE and bedding.

Globally and locally, LCAs are giving us insights on how the healthcare industry can reduce it's environmental footprint and decarbonise healthcare – one decision at time.
Making sustainable decisions is not always clearcut and LCAs show up differences between countries.
An Australian study in 2017 found that switching to reusable anaesthetic equipment provided significant cost savings and reduced waste going to landfill.
But doing so increased carbon emissions due to electricity consumption for washing and sterilisation.
In Europe, where renewable energy dominated at the time, reusable anaesthetic equipment would have achieved a reduction in carbon emissions by 84 per cent.
In 2024, the increasing use of renewable energy in the Australian electricity grid brings us more in line with European emissions savings, which makes the case for reusables in Australia even stronger.
Sciences & Technology
Sustainability needs women and girls in science
In Victoria, the State Electricity Commission (SEC) will supply 100 per cent renewable energy to all public hospitals by 2025, which means the carbon impacts from washing and sterilisation will fall even further.
The good news for the hospitals and politicians overseeing health budgets is that sustainability makes good financial sense. LCAs highlight where efficiencies can be made, reducing both carbon emissions and financial costs.
The provision of healthcare indirectly creates harms to the health of people in the future, with those harms more likely to fall on people living in low- and middle-income countries.
For equality and intergenerational equity, healthcare needs to do its part to rapidly decarbonise while also ensuring no harm comes to patients today.
The decarbonisation of healthcare requires a multidisciplinary approach – from clinicians and other healthcare workers, policy makers, health administrators, procurement departments, engineers, health economists and environmental specialists.

This work is already happening across all University of Melbourne-linked healthcare and biomedical research organisations, with healthcare workers and management leading change across the hospital system.
By choosing reusable gowns and other PPE equipment, improving hospital energy efficiency and providing high-value-low carbon clinical care (like non-operative approaches instead of surgery) while avoiding low-value and high-cost care (like unnecessary pathology tests) – then overall emissions can be driven down.
The Healthcare Carbon Lab will be an important part of local decarbonisation but will also provide detailed LCA data for national and international use.
This means healthcare providers can make scientifically informed decisions to support their decarbonisation journeys.