
Health & Medicine
The future of Australia's doctors

New research finds that general practitioners and other specialists are feeling the stress – not just from COVID-19, but also the broader economic fallout
Published 16 July 2020
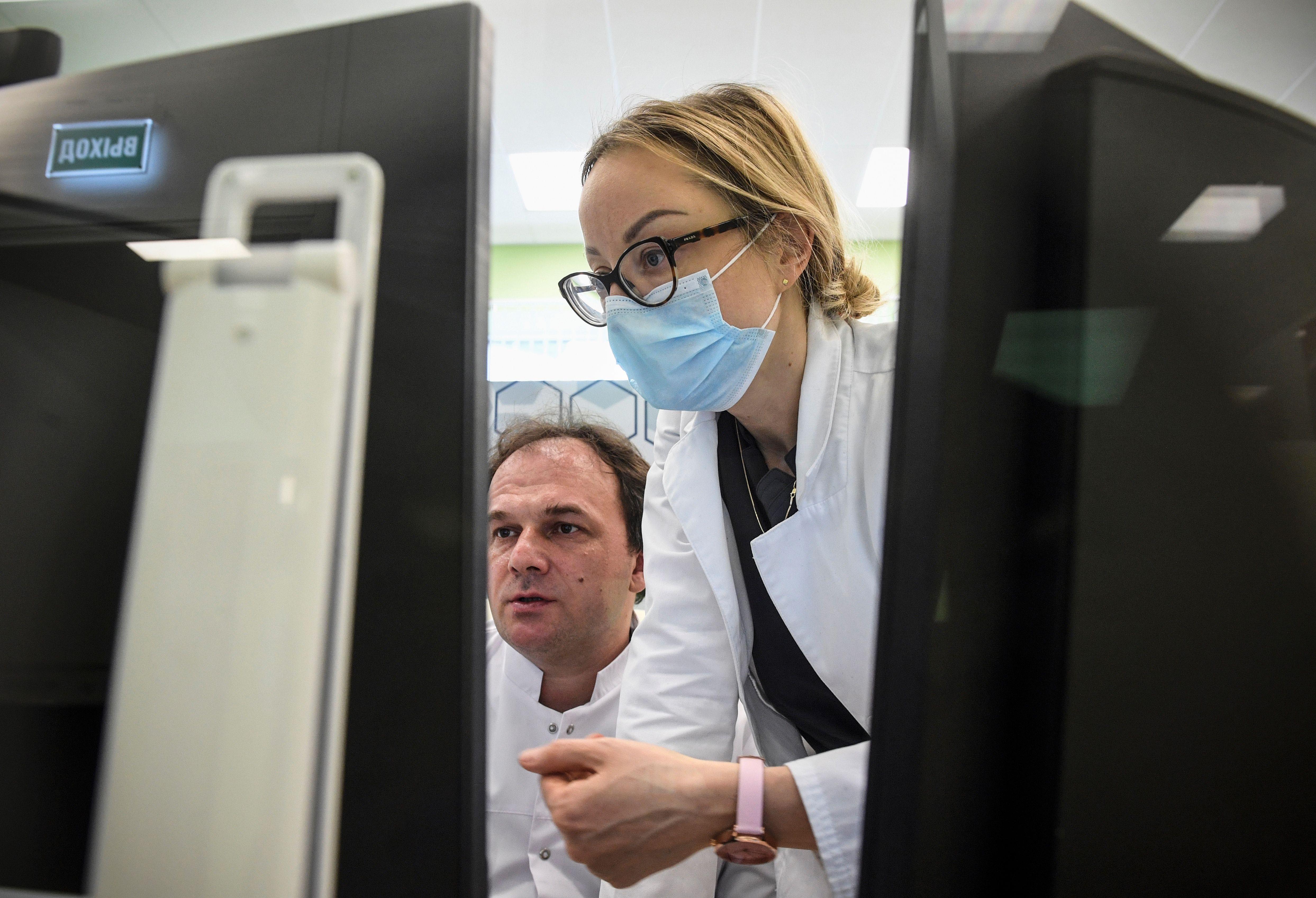
Australia’s health workforce has been at the frontline in dealing with the COVID-19 pandemic. They have placed themselves and their families at risk in helping others.
But at the same time, health practitioners are having to adapt to significant changes in how they provide care amid ongoing uncertainty – not just about the pandemic itself, given Melbourne has been been forced into another lockdown – but also how the pandemic will shape the longer term future of healthcare.

For example, many surgeons lost work when non-urgent elective surgery was suspended during April and May 2020.
The pandemic also weighed on the demand for wider healthcare services as social distancing restrictions discouraged people from leaving home, and public fears of contracting or spreading the virus kept people away from health facilities.
Job losses and uncertainty throughout the community has also put increased financial pressure on household budgets, which can be expected to reduce the affordability of out-of-pocket payments for healthcare services.

Health & Medicine
The future of Australia's doctors
So, how are our general practitioners and medical specialists faring?
During May, we conducted a special national survey to examine the impact of the COVID-19 pandemic on GPs and specialists, with a focus on those working in private practice.
The longitudinal Medicine in Australia: Balancing Employment and Life (MABEL) COVID-19 Short Online Survey (SOS) was completed by over 2000 GPs and other specialists.
The results suggest that the sector has been quick to adapt to providing telehealth services during the pandemic, which has the potential to become a permanent shift.
But at the same time, the pandemic has radically altered the way medical care is being delivered, led to significant financial challenges for doctors in private practice, and increased stress for many.
Our results suggest that there was a more immediate and consistent fall in the use of healthcare for non-GP specialists because of the ban on non-urgent elective surgery.
Though non-GP specialists were more consistently affected compared to GPs – where there were more mixed effects on workload – the ban is now lifted and there is evidence that the private non-GP specialist sector may bounce back more quickly compared to GPs, given the backlog.
Health & Medicine
The science behind the search for a COVID-19 vaccine
For both GPs and other specialists, the introduction of new Medicare funding for telehealth consultations helped protect doctors and patients from infection, and also helped to stem the fall in the use of healthcare by patients.
Our data shows that more than one third of all consultations were provided by telehealth in April and May 2020, with almost all GPs using it and around three-quarters of non-GP specialists using it.
The use of telehealth was lower among GPs operating in solo practice, as well as among GPs in the most disadvantaged areas and in rural areas. There were no differences by GP age or practice size in the take up of telehealth.

Over 95 per cent of GP telehealth consultations were by telephone rather than video.
This is a concern given doubts over the the appropriateness of relying on telephone consultations for some areas of care. The results suggest that more effort needs to be put into encouraging a greater use of video consultations.
Around 84 per cent of doctors think that telehealth should be permanently funded by Medicare.

Health & Medicine
The world needs nurses now more than ever
Telehealth is likely to create a structural shift in how health care is delivered, though this depends on how this temporary funding will continue into the future. It’s very convenient for patients, and could lead to an increased demand for GP services as people no longer need to take as much time off work to ‘visit’ a doctor.
The rapid changes to patient numbers and telehealth in April and May 2020 have significantly reduced incomes for some practitioners, with 65 per cent of GPs and 83 per cent of non-GP specialists reporting a fall in monthly income.
Almost one-third of surgeons and anaesthetists reporting a fall income of 50 per cent or more, which mainly reflects the suspension of elective surgery.

Around 30 per cent of all doctors reported feeling very or moderately financially stressed about their private practice. Reported financial stress was particularly prevalent among larger non-GP specialist practices.
GPs in urban areas or in the most affluent areas were more likely to report a fall in income and experience financial stress and mental stress. These practices were worst hit probably because they were more likely to charge higher fees and bulk bill less before the pandemic. So, the substitution of face-to-face consultations for less profitable bulk-billed telehealth consultations may have hit them hardest.

Health & Medicine
3D printing medical equipment for COVID-19
Falls in patient numbers were also higher in urban and more affluent areas compared to rural and more disadvantaged areas.
Some 18 per cent of GPs and 51 per cent of non-GP specialists reported that their practice had applied for the Federal Government’s JobKeeper payment subsidy, and this was more likely in urban rather than rural areas.
A small proportion of GPs (5.6 per cent) and non-GP specialists (8.4 per cent) thought their practice might be sold or closed in the next six months.
These respondents were more likely to be from smaller GP and non-GP specialist practices, and or be older non-GP specialists. It may be that for practitioners nearing retirement, the pandemic may have brought these decisions forward.

The longer-term financial health of the sector depends on the mix of services between bulk-billed telehealth and full-fee, face-to-face consultations going forward, and how practices adapt in the context of recent and future changes in Medicare funding around telehealth.
In addition, extended economic hardship in the wider community may cause a longer-term decline in demand for private medical care and private health insurance. This was already a key issue before the pandemic, and is particularly an issue for non-GP specialists in the private sector.

Health & Medicine
How should medical students respond to Covid-19?
Unsurprisingly, the survey reveals high levels of stress among doctors.
The significant changes in the mix of care being provided, the increased risk to doctors’ own health and the high levels of uncertainty about revenue flows caused by the COVID-19 pandemic are having an impact on doctors’ stress levels.
Around 60 per cent reported feeling more stressed than usual, with those who experienced a fall in income more likely to report feelings of stress.
Significant proportions of non-GP specialists (almost a half) and GPs (around one-third) were dissatisfied with access to personal protective equipment during the pandemic, which was associated with increased feelings of stress.

The pandemic and its consequences have accelerated a number of pre-existing trends in the healthcare sector and among the medical workforce, including the increased use of telehealth and the lower growth in the use of private medical care.
These changes present challenges, but also new opportunities for improving the delivery of medical care in Australia for the benefit of patients.
How these changes influence the quality, costs and access to healthcare in the future is a key issue going forward as everyone adjusts to the ongoing challenges caused by the pandemic.
Banner: Getty Images