
Politics & Society
Patients and the data breach notification maze

Clear processes are needed for recording medical consultations. New research aims to help patients and providers to record openly
Published 30 May 2022
Seeing a health professional is an essential part of the healthcare journey, whether it is in person or through the now common telehealth service. During these relatively short interactions, a lot of important, sometimes life-changing information is shared.
However, research has shown that people forget most of what they are told in healthcare appointments. This means that they might not understand their illness very well or might find it difficult to remember important health or treatment information like what dose of medication to take or how to prepare for surgery.

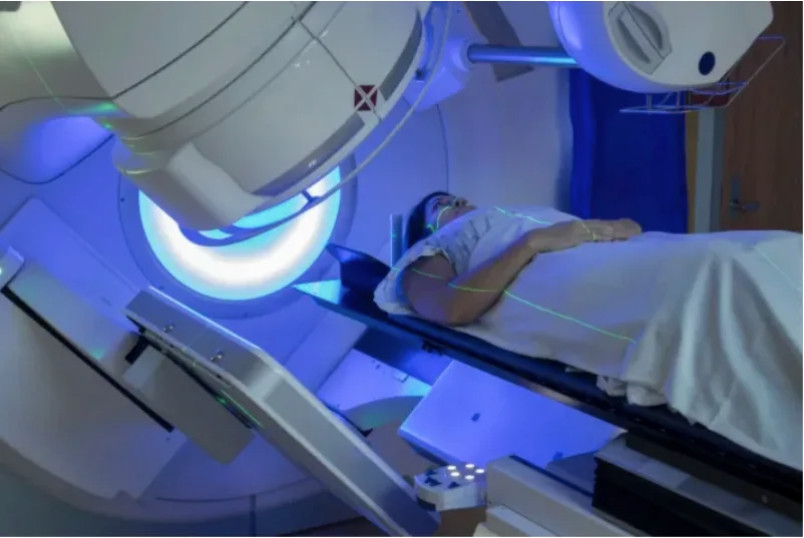
This is especially true when people are being told upsetting news, including receiving a diagnosis of cancer or another serious condition, or must undergo significant treatment like a major operation. Not having a clear memory of what was discussed can limit people’s understanding and ability to participate in important decisions about their treatment and care.

Politics & Society
Patients and the data breach notification maze
From over thirty years of research, we know that people find it helpful to be able to later listen to an audio recording of their health consultation. Importantly, recordings work well to improve people’s recall and understanding of the information they were given by the health professional.
Being able to play a recording of a consultation back, for instance, to close family members, or even to another doctor such as the patient’s GP, also means that those around the patient can understand, help and support them better.
Health professionals also value and support the use of consultation recordings for the benefits it can provide to their patients. Recording has been found to enhance the patient’s trust in the health professional and makes them feel more supported and more satisfied with their care.
To understand more about people’s preferences, specifically how and why people record their medical appointments, our team of law and health researchers has launched a new short and anonymous survey.
The results will help explain why some people are making recordings when they see their doctor or another health professional, who they want to then share these recordings with, and how. Our goal is to gather information on this often-hidden practice for the first time in Australia, to help inform the design of new policies and recording technologies.
Previously, studies of consultation recording used cassette tapes and clunky technology. Now, smartphone voice recorders make it easy for anyone to record their healthcare consultation, and some health professionals encourage their patients to do that for the reasons above.

Health & Medicine
Widening access to clinical trials
There are also new apps designed to enable patients to record their appointments, many of which include extra functions including automatically generating written transcriptions of the consultations or highlighting key medical terms and linking to reputable sources of health information.
At the Peter MacCallum Cancer Centre they are developing the SecondEars app to make it easier for patients to record their visits. It uploads a copy of the recording to the patient’s electronic medical record before the patient can listen back to it.
It is also known, from anecdotal evidence and through research conducted in the United Kingdom and the US, that people often make recordings of their consultations without telling the health professional. For instance, 26 per cent of people completing one survey in the UK reported that they had recorded a visit with a health professional covertly, or they knew someone who had.
While covert recording might still provide the benefits to patients we mentioned earlier, it could be seen as unfair as it risks undermining the doctor-patient relationship and makes some health professionals concerned that patients might be wanting to ‘trip them up’.

Although research overseas has explored how often people have recorded their consultations (both covertly and openly) and whether they want to in the future, the picture in Australia is much less clear as no one has collected this information before.

Health & Medicine
Improving cancer care through good communication
This means that efforts made by health services such as the Peter Mac, or even by individual health professionals to promote consultation recording, are ‘flying blind’. They don’t have the information they need to help design new recording technologies and the policy framework to support them.
Our new survey aims to fill this gap by seeking as many people as possible to complete it and share their current practices and preferences about healthcare recording.
But as well as technological considerations, there are lots of legal and ethical questions about recording consultations. Concerns about these, and about the rights of health professionals and patients to make and share recordings, might make people hesitant.
This has led us to undertake other research and wide-ranging conversations across the spheres of law and regulation, clinical practice and with the involvement of patients.
Our work has looked at what doctors and patients think about a consultation recording app and what Australian law allows and requires – especially in terms of consent to make a recording and to play a recording to others.

Our legal research found that relevant law in Australia is complex, with significant differences between jurisdictions, making it all the more important that new technologies to enable consultation recording are explicit about the terms and conditions of the recording and its later use.
Our goal is for this engagement and research to bring changes in policy and practice so that more patients and health professionals can receive the known benefits of consultation recording. But we need to do this in an ethical way and address the needs and concerns of everyone involved.
Healthcare consultation recording is the focus of an event on 1 June at the University of Melbourne. The event will launch a new University initiative, the Collaborative for Better Health and Regulation. It consists of a forum to bring together the perspectives of clinicians, lawyers, regulators and patients. Members of the public are welcome to attend this event.
Banner: Getty Images