Oxygen machine powers on to save lives

How a physicist and a global health expert joined forces to give the breath of life to critically-ill children in hospitals without a secure source of electricity
Published 7 October 2015
How does a team made up of theoretical and particle physicists and medical scientists from the University of Melbourne solve a problem which kills 1.5 million kids a year?
The problem is that blackouts in low and middle-income nations stop oxygen generators in their tracks, potentially leading to the death of children with pneumonia, the number one killer of children under five worldwide. Worse, many small health facilities have no access to electricity at all.
Pneumonia kills one child every 30 seconds. Even if a child suffering from severe pneumonia is on antibiotics, without a steady flow of purified oxygen their lungs struggle to cope and the condition often becomes fatal.
But a cross-faculty partnership at the University of Melbourne might just have come up with some creative and (importantly) low-cost ways to remove the nitrogen that makes up 78 per cent of the air, leaving purified oxygen to go to the patient.
New approach to solve old problem
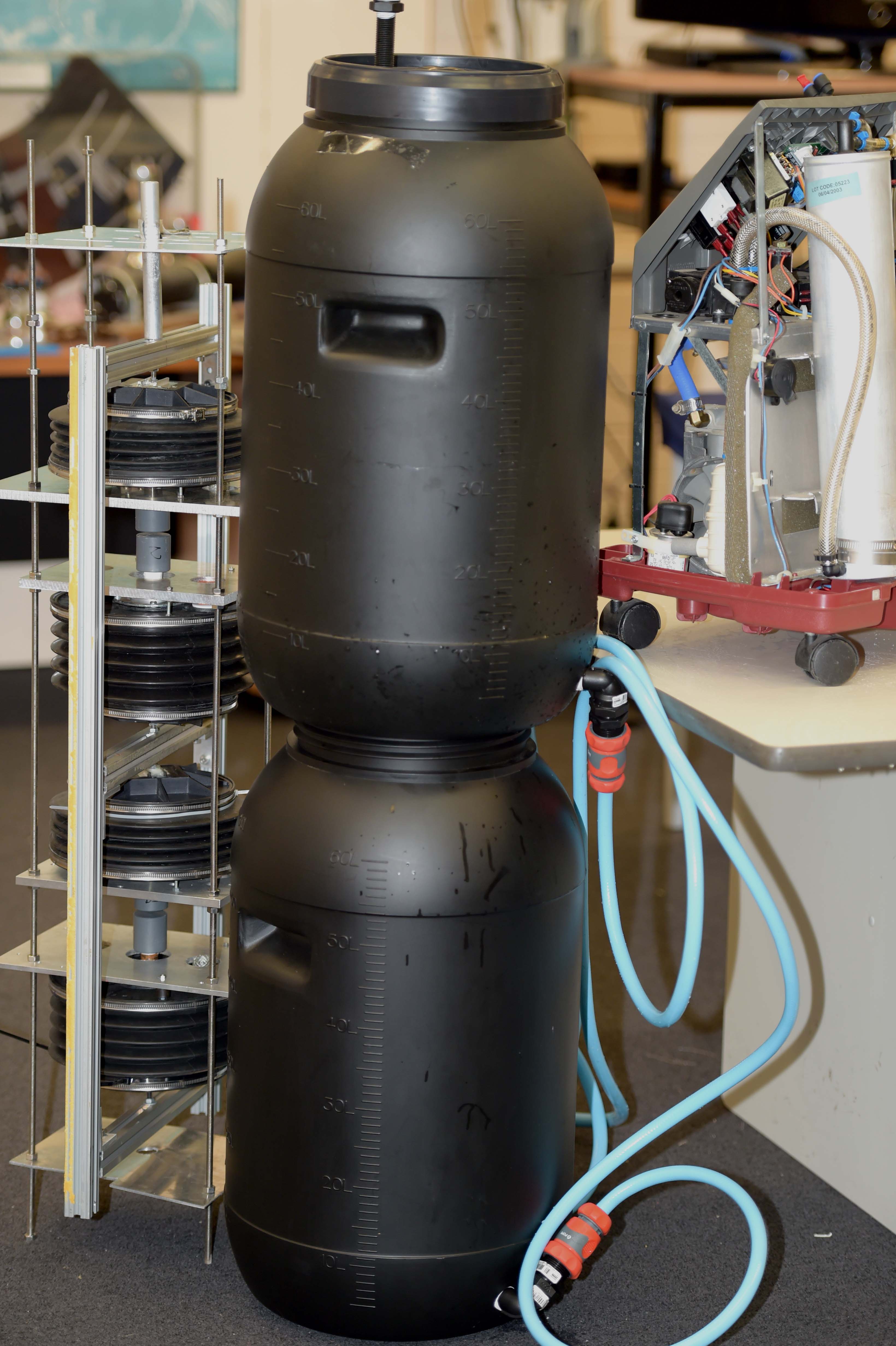
Where there is electricity, they build on existing oxygen concentrator technology by storing some of the oxygen locally at low pressure, ready to come instantly online and ensure a steady supply whenever the electricity fails.
The solution for places with no electricity comes straight out of left field: a new approach to concentrators that uses a vacuum created by water running in a nearby stream or river.
The key with both solutions is their basis in solid physics – both represent absolutely the lowest possible energy cost, which translates into lower running costs and greater sustainability in resource-poor settings.
Providing oxygen in the smallest hospitals and health centres has the potential to reduce child pneumonia mortality rates in these settings by up to 30 per cent.

For Associate Professor Roger Rassool and his team from the School of Physics, the collision of minds with Associate Professor Jim Black, from the Nossal Institute for Global Health, came at a symposium a few years ago.
The two Associate Professors were old sparring partners from luncheons at the University of Melbourne’s University House staff club, but they had one thing in common – a commitment to helping disadvantaged children.
“If you’ve ever been to lunch at the Club, there are always arguments and discussions and everyone knows everything,” Associate Professor Rassool says.
Their friendship may have remained at the theoretical discussion stage if not for a symposium held at the Nossal Institute for Global Health a couple of years ago.
Associate Professor Black, whose expertise is in health in low-income countries, takes up the story: “We brought speakers from the world of healthcare in low-income countries to an audience of engineers, physicists and other ‘technical’ people.
Looking for a novel solution
“The clinicians outlined issues they considered important and which seemed to need technical solutions, in the hope that someone in the audience might have a novel solution.”
Among the half-dozen speakers was a leading childhood pneumonia researcher mostly working in Papua New Guinea at the time.
“He explained how much potential there is to improve pneumonia outcomes by supplying oxygen in small health facilities, but pointed out that such health facilities have unreliable electricity supplies, so that standard oxygen concentrators may switch off at critical times, putting lives at risk during electricity blackouts.”
Even worse, they tend to burn out as a result of voltage fluctuations, giving them very short working lives. He asked the technical audience to find a cheap way to provide reliable electricity in remote settings.
In the audience was Associate Professor Rassool and post-doctoral colleague Dr Bryn Sobott, who went away to think about it.

“Being physicists they went right back to basics, looking at how concentrators work and what the actual energy requirements are,” Associate Professor Black says.
“They came back to me (as organiser of the symposium) and asked if the question is really about electricity - in fact what a concentrator needs is compressed air, so they re-phrased the question as: ‘How do we build a low-cost air compressor that does not need reliable electricity?’
“Re-imagining the problem in this way opened up a wide range of possibilities, and we worked through four or five really imaginative possibilities over the next couple of years. Yes, years - we were all working on this in our ‘spare time’ without a grant or other funding.”
Associate Professor Rassool says the breakthrough for him came when he realised the problem was not about power, but one of pressure.
“The eureka moment was when we realised we didn’t have to use electricity to make oxygen.
“There was also a physics moment when we realised vacuum was pressure – a lack of pressure that could be used, by flipping the process to vacuum-based we could use the vacuum to suck the nitrogen out of the air.”
The rigs are not small – one takes up about half a shipping container – and locals will have to be trained not only to use the equipment, but also to monitor patients’ blood oxygen levels to ensure it is working properly.
And the cost? “As low as possible,” says Associate Professor Black.
The team now has a prototype operating in Gippsland; Associate Professor Rassool has gone to Uganda for initial fieldwork and Associate Professor Black has been to Mozambique negotiating partnerships in preparation for trials.
Both consider it vital to work closely with local researchers and health workers in refining the designs and making sure they fit well into the health facility’s workflow.
“The important aspect of the meeting of Jim and our team is we both have an interest in disadvantaged people and we aren’t wedded to our own disciplines,’’ Associate Professor Rassool says.
“We aren’t wedded to pushing our own solutions but are galvanized to an outcome; that enables us to play the ball, not the person when we argue.
“We both bring complementary and overlapping skill sets. Some of our team are extremely computer literate. Some are very hands on and some have medical skills.”
So what’s next? “So far we have been making contacts with locals and young people we can train up to run our systems. We are hoping to get working systems on the ground in November-December and a fully operational system in the New Year.”
The team has a sobering key performance indicator.
“Our KPI is how many lives have we saved,” Associate Professor Rassool says. “You can’t argue with it. It’s confronting mortality and trying to not get too personal with it.”
Rewards of the job
He says working in places like Uganda can be hard. “You stand in these environments and say: ‘I can solve these problems.’ But there are hundreds of thousands of problems.”
There are rewards for this labour of love too.
“We have been inundated with warmth by the local communities there. They are so receptive. It is embracing and it keeps your spirits up.”
The team has received $100,000 from the Bill and Melinda Gates Foundation via its Grand Challenges Explorations Grants program and a $250,000 Seed grant from Grand Challenges Canada to prototype new technology, with a chance to receive a further $1 million once it is proven.
The ultimate aim is to establish a startup in Melbourne with strategic partnerships between the University of Melbourne, industry and community, to form the manufacturing capability in Australia. There is a long road ahead but the potential rewards – in terms of avoiding unnecessary childhood deaths – are great.
Banner Image: Pixabay

