Health & Medicine
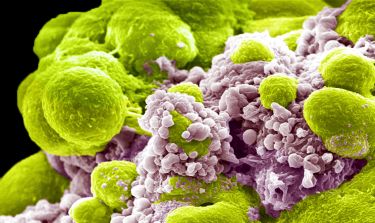
A smarter way to deliver drugs

Throughout her career, Professor Mei Krishnasamy has worked to improve the evidence base for cancer nursing care, particularly for people with rarer cancers
Published 3 February 2019
I trained at the University Hospital of Wales in Cardiff in the UK. After training I worked as a staff nurse Velindre Cancer Centre in Cardiff, where I cared for people diagnosed with head-and-neck and lung cancers – these diagnoses reflect the mining industry in the area.
My passion for advocating for and enhancing the nursing care of these patients has never left me. They made me realise the importance of looking out for those patients who, because of issues like poverty, low health literacy and malnutrition, are at risk of poorer outcomes.

I knew I would never leave oncology. I knew it within 12 months of starting at Velindre Cancer Centre. After that I moved to the John Radcliffe Hospital in Oxford where I worked as a primary nurse in a new dedicated clinical trials unit. It was here I developed my fascination for clinical trials and appreciation of the critical importance of creating opportunities for patients to take part in all kinds of clinical research.
Along with my husband and three small children, I came to Melbourne in 2003. I was fortunate to work alongside Professor Sanchia Aranda in the Department of Nursing and Supportive Care Research (DNSCR) at the Peter MacCallum Cancer Centre (PeterMac). After three years, we went back to the UK, but 18 months later we were back. I re-joined the PeterMac and became the Deputy Director of the DNSCR working to build clinical nursing research skills and opportunities.
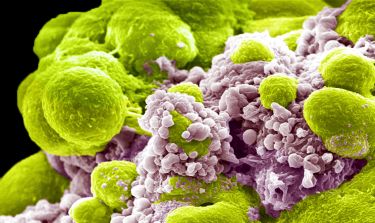
Health & Medicine
A smarter way to deliver drugs
Then in 2016, I joined the Department of Nursing at the University of Melbourne as the inaugural Chair in Cancer Nursing. The role was brand new, there to be developed, to do what I wanted with. When I started, there was just me. I’ve now got a team of 16 people who work across 11 research projects. Later that year I was appointed Research and Education Lead for Nursing across the seven clinical partners of the VCCC (Victorian Comprehensive Cancer Centre).
To many, our work may sound simple, but its impact and reach are huge. What’s remarkable for us is hearing people say, ‘I know my time is limited but what I need is help to live as well as I can for as long as I can’. Asking people regularly if they need help, what help they need and who from, makes a big difference to their cancer outcomes.
So, we’re working to refresh Victorias’ approach to the integration of supportive cancer care as part of a state-wide study funded by the Department of Health and Human Services. We are working to understand how we integrate support into day-to-day care for all people affected by cancer.

Patients with rare or less common cancers can lack the advocacy people with more common cancer benefit from. So, to address these challenges, our projects target functional, physical, social and emotional challenges that accompany a diagnosis of cancer.
For example, in one of our co-design studies, we’ve worked with people affected by pancreatic cancer, which still has very poor outcomes. Consulting with patients, carers and clinicians we’ve developed a web-app that includes advice and support that people need, when they need it. Patients and carers tell us it’s just what they wanted.

Health & Medicine
Putting cells through their paces
We’re now working on a project focusing on multiple myeloma. This is a cancer of plasma cells in the bone marrow – it’s incurable and as it progresses, people often experience complex symptoms. The project, which was recently funded by the Nurses Board of Victoria Legacy Limited Grants, aims to map patterns of care for metropolitan and regional patients with multiple myeloma once they have completed an initial component of therapy.
Working with specialist myeloma doctors and nurses from PeterMac and Myeloma Australia, we want to find out how to leverage a national network of specialist myeloma nurses. This means regardless of where patients with multiple myeloma are, they will have access to expert nursing consultation.
From the point of diagnosis, people must have the care, support, information and knowledge they need to live as well as possible for as long as possible. The value of our work is measured by its impact on the lives of people in the ‘here and now’ – as well as its contribution to the people yet to be affected by a diagnosis of cancer.

We’re still very much at the beginning of growing the cancer nurse research agenda. It’s exciting that we have an opportunity to build what will be a leading program of international cancer nurse-led research. The investment from the University and the VCCC in my role gives us a strong start to drive the quality and safety of nurse-led care for all Australians affected by cancer.
- As told to Cheryl Critchley
Banner: Getty Images