
Health & Medicine
The long-term benefits of controlling your asthma

Researchers have uncovered a molecular pathway that can be blocked to potentially prevent the destructive inflammation of chronic obstructive pulmonary disease, a major worldwide killer
Published 8 May 2018
Sometimes you can have too much of a good thing – even infection-fighting white blood cells.
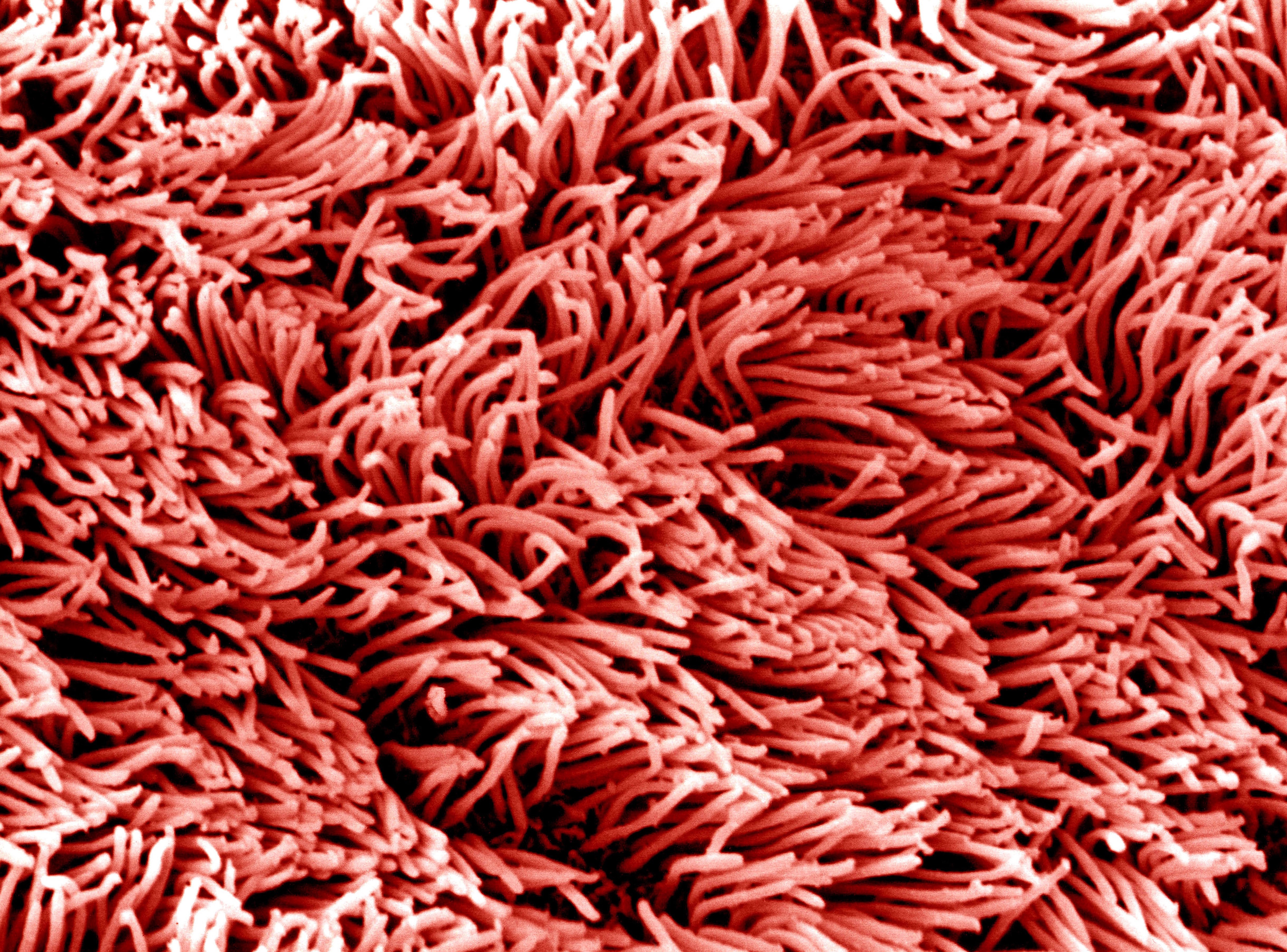
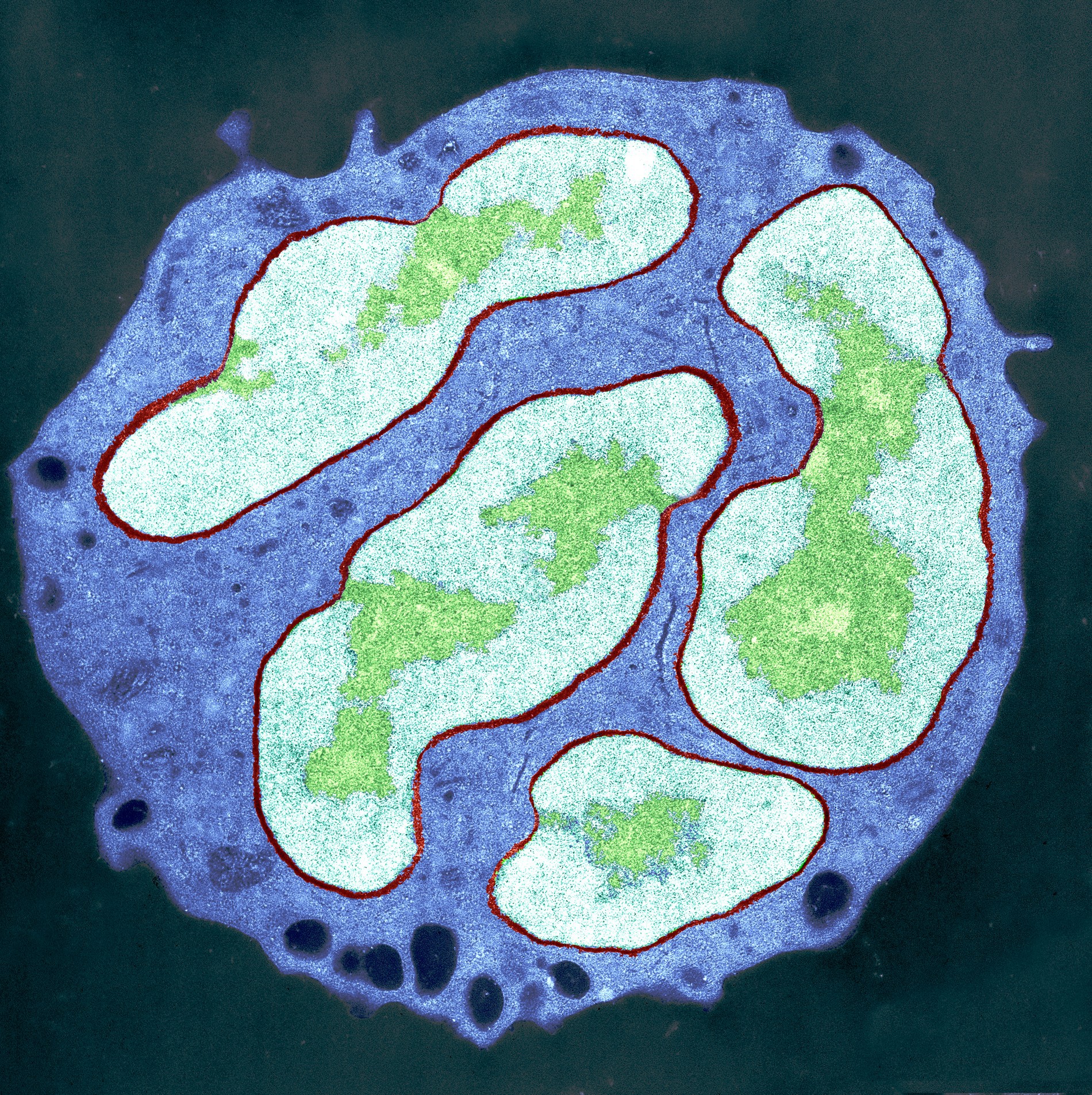
People with emphysema, or Chronic Obstructive Pulmonary Disease (COPD), have their lung tissues slowly eaten away by chronic inflammation, and the major culprits are specialised white blood cells called neutrophils and macrophages. While adept at combating lung infections, these cells can also attack the elastic fibres of the lungs leaving people struggling for breath and prone to chest infections.
There is no cure, and while abnormally high levels of white blood cells have long been associated with emphysema, scientists have struggled to find an underlying cause that drugs could effectively target.
But a team of Australian scientists from Monash University and the University of Melbourne have discovered that COPD – and the co-associated medical problems that afflict patients – can be stopped by directly “blocking” a critical protein known as G-CSF that ordinarily works to stimulate the production of white blood cells.

Health & Medicine
The long-term benefits of controlling your asthma
The study, published in The Journal of Clinical Investigation, opens the way for what could be the first treatment that actually prevents the disease from progressing, as well as providing a new ‘biomarker’ to screen people for much earlier diagnosis.
“We found elevated levels of G-CSF in mice with COPD, and when it was eliminated, the excessive numbers of white blood cells in their lungs were markedly reduced and the lungs themselves no longer became diseased,” says senior author of the study, immunologist Associate Professor Margaret Hibbs from Monash University.
“Nothing previously has proved to be effective in treating patients with COPD, which is why this finding is so exciting. We can now attempt to target this protein.”
The genesis of the research goes back to a major international study, published in 2012, that highlighted a strong association between COPD and elevated numbers of white blood cells. When they looked at the results, Associate Professor Hibbs and her long-time friend and collaborator Professor Gary Anderson, director of the Lung Health Research Centre at the University of Melbourne, were intrigued.
When follow up studies found that high white blood cell counts were also associated with the damage COPD does to other tissues, like the heart, muscles and bones, they decided to investigate.
“That really cemented in our minds that the white blood cells were a fundamental clue to follow,” says Professor Anderson.
They formed a team of medical researchers with diverse expertise, including study lead author and immunologist Dr Evelyn Tsantikos from Monash University, and carefully evaluated the effects of blocking G-CSF using mice genetically modified to be prone to COPD symptoms.

Health & Medicine
Exercising with lung cancer
“When we blocked G-CSF, the effect was absolutely striking,” says Professor Anderson. “It prevented not only the emphysema, but also the wider medical problems, whether it be the heart, muscles or bone. We realised we had uncovered a potential pathway for treatments.”
COPD kills about 3 million people each year, making it the third most common cause of death worldwide behind heart disease and stroke. Globally there were an estimated 251 million cases of COPD in 2016, while in Australia over 1.45 million people have some form of COPD.
But narrowing down an apparent cause of COPD in mice to G-CSF doesn’t mean it works the same way in humans. Before they could contemplate moving into clinical trials the team needed to know if the elevated levels of G-CSF in mice with COPD was replicated in patients suffering from COPD.
To investigate this critical point, they presented their findings to clinical respiratory researcher and director of clinical training at the Royal Melbourne Hospital, Associate Professor Lou Irving.
He immediately appreciated the implications and facilitated access to a cohort of respiratory patients, with and without COPD, who volunteered to be sampled as a normal part of their care. As the team suspected, they found that COPD in humans was correlated with high levels of G-CSF.
“We now have a very good case that we have indeed found a mechanism not just for preventing emphysema and chronic bronchitis in the lungs, but also for preventing the damaging medical conditions associated with it,” says Professor Anderson.
“There are several safe ways to reduce G-CSF in people and this concept can now be tested in human clinical trials.”
G-CSF can be blocked using already established antibodies. By simply adjusting the dose of any eventual therapeutic, Professor Anderson says clinicians could be able to maintain the infection-fighting ability of these white blood cells while preventing the collateral damage that leads to COPD.
“We aren’t proposing to eliminate G-CSF but to keep it at levels within the normal range. That way we can preserve the normal defence function of these white blood cells but stop them from becoming over-aggressive to lung tissue and other body tissues.”
According to Professor Hibbs, “this would be the first ever strategy that would not only treat the lung disease but the co-associated medical conditions at the same time.
“If successful, this has the potential to benefit the millions of people who suffer this terrible disease.”
Banner Image: Internal architecture of the trachea and lungs, 3D printed in Frosted Ultra Detail plastic. Picture: Dave Farnham/Wellcome Collection