Health & Medicine
The science behind the search for a COVID-19 vaccine

Finding existing drugs that are effective against COVID-19 is our best bet toward treatments, and the US buy-up of Remdesivir supplies highlights how urgent the race is
Published 8 July 2020
The growing outbreak of COVID-19 cases in Melbourne is a stark reminder that the pandemic is far from over in Australia, and with cases continuing to rise alarmingly in places like the US, Brazil and India, efforts are intensifying into finding a drug that can help combat the potentially deadly disease.
While we aren’t yet on the cusp of a solution that decisively stops the SARS-CoV-2 virus that causes COVID-19, drugs may prove to be an important tool in treating or preventing SARS-CoV-2.

On Monday June 29, American biopharmaceutical company Gilead Sciences announced its price for Remdesivir – one of the first antivirals to show effectiveness against the coronavirus in published human trials. Within days, the USA had bought up the remainder of Gilead’s available global supply.
The Australian National COVID-19 Clinical Evidence Taskforce has released tentative advice that Remdesivir “may be considered” in some COVID-19 cases, but cautions about the limited evidence for its efficacy so far. Further trials will soon begin for an inhalable version of the drug shown to shorten the average recovery time of hospitalised patients.
Health & Medicine
The science behind the search for a COVID-19 vaccine
Simultaneously, efforts continue to explore other treatment regimes, and combinations of existing drugs, that could help treat COVID-19.
Here we ask Associate Professor Stuart Ralph and Dr Craig Morton from University of Melbourne’s School of Biomedical Sciences to explain how anti-viral drugs work and go through the different drug candidates that may help treat COVID-19.
Viruses lack the full molecular apparatus to replicate themselves, so instead they hijack the machinery of the host cells they infect in order to make more copies of themselves. So, while bacteria and parasites typically need thousands of genes to construct their own molecular machinery to replicate themselves, viruses are much simpler and can get by with far fewer genes. SARS-CoV-2 only has a few dozen genes, while some other viruses have just three or four.
This simplicity is the reason antibiotic-style drugs can’t be used to treat viral infections. An antibacterial drug can be developed to combat a bacterium by jamming that mechanism it uses to replicate itself. But because a virus uses our own cells to replicate, drugs like these can end up hurting us more than the virus.
Another problem is that viruses can be very different from one another. For example, a human has more genetically in common with a horseradish than do the two viruses that cause influenza and chickenpox. This means finding a drug that can target a large variety of viruses, like antibiotics do for bacteria, is incredibly challenging.

Health & Medicine
Q&A: Dexamethasone and COVID-19
Viruses are generally picky about the type of host cell that will offer a hospitable environment for them to exploit. They feel their way across the surface of a host cell to determine if it has just the right combination of proteins and sugars that identifies it as an appropriate temporary home.
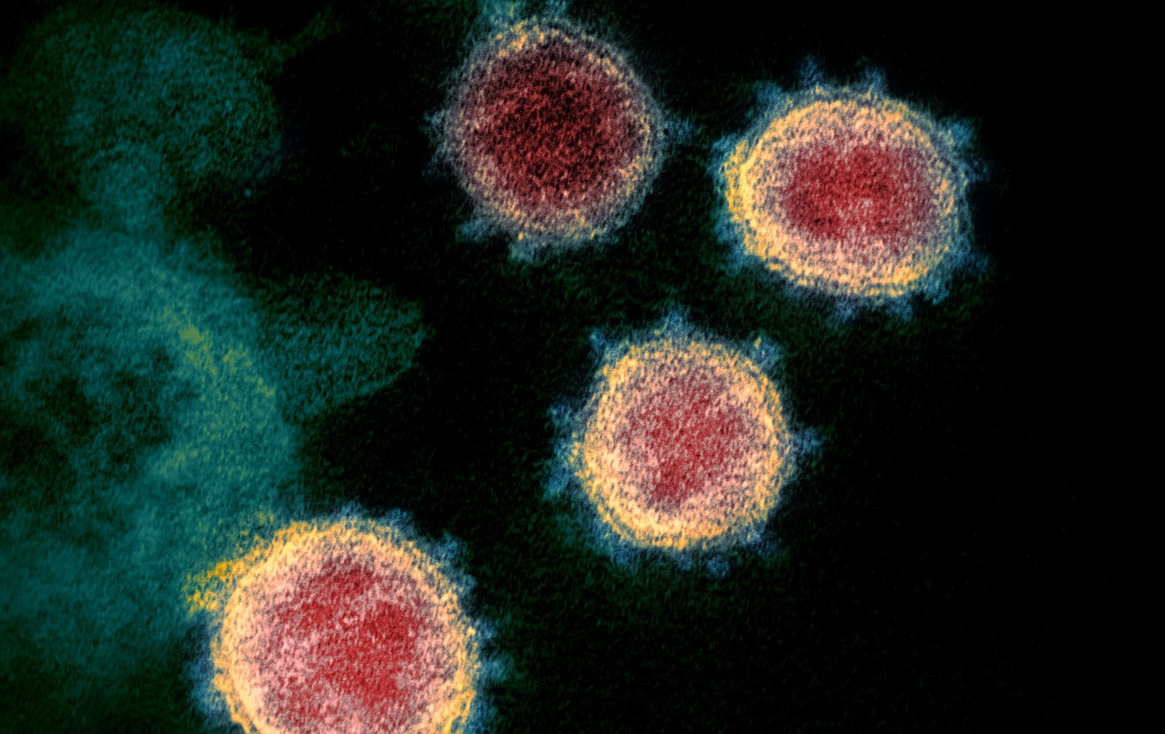
Coronaviruses are spheres with dozens of spikes that stick to the surface of a cell it is invading. The spike protein looks for an enzyme called ACE2 that is on the surface of several different types of human cells and which normally plays a role in regulating blood pressure. When the spike binds to ACE2 it triggers the fatty membrane that surrounds the virus to fuse with the membrane that surrounds our cells so that the viral contents spill into our cells – a bit like soap bubbles colliding and then merging in the bath.
Scientists are working to identify drugs that can interfere with this process, either by blocking the interaction between the spike and ACE2 directly, or stopping the spike proteins from triggering fusion of the virus with the human cell.
The controversial drug Hydroxychloroquine likely works by interfering with this process, and Australian trials are underway to test if it has a role in preventing COVID-19.

Some researchers have also generated designer antibodies (infection-fighting proteins in our bodies) that may be able to block a coronavirus from recognising a host cell and so stop the virus from entering. These appear to be effective in animal models, and we await human clinical data.
The same strategy of blocking viral entry has been used successfully to develop a drug called Maraviroc and an antibody treatment called Ibalizumab that are each effective against HIV, validating this general approach for making anti-viral drugs.

Health & Medicine
What actually works for anxiety and depression?
Once inside a host cell, a virus needs to make multiple copies of itself to proliferate. Different types of viruses use different ruses to trick the host cell into making these copies. Coronaviruses, for example, use some of their own molecular machinery to copy their ribonucleic acid genome, and this process has been exploited using a range of drugs that poison the viral replication machinery.
Several of these compounds are now being advanced as potential COVID-19 drugs. One of these is Remdesivir – originally developed to treat Ebola.
Viruses also need to use a collection of other building blocks to replicate themselves, including proteins, fats and sugars. New drugs that inhibit the virus from processing these other building blocks inside the host cell have recently transformed the treatment of important viral diseases, including hepatitis C and HIV.
Drugs that work on this basis, such as the HIV drug combination Kaletra™, have been trialled against COVID-19, but at least one large study found no benefit to this drug.

The final part of a replication cycle is when the virus’ progeny exit the host cell to seek out other new cells to infect. Sometimes this causes an explosion of the host cell left behind. However, coronaviruses hijack the cell’s export machinery to exit without immediately destroying the host cell.
A number of important drugs, like the well-known anti-influenza drugs Relenza™ and Tamiflu™, work by stopping this active release of the virus from the host cell. Unfortunately, the machinery that influenza uses to do this differs from coronaviruses, and these drugs have proved ineffective against COVID-19.

Business & Economics
Who’s hit hardest by the COVID-19 economic shutdown?
Some of the patients who have died from COVID-19 suffer from an overreaction of their body’s immune response to SARS-CoV-2 virus. A large UK study reported that the steroid drug Dexamethasone, which is an immune suppressant and anti-inflammatory, reduced mortality of COVD-19 patients on ventilators by around one third, but this trial is yet to be peer reviewed.
The Australian National COVID-19 Clinical Evidence Taskforce advises that some COVID 19 patients receiving oxygen might benefit from this drug but are awaiting more results from the Dexamethasone trial before making a more general recommendation for an Australian setting.
Discovering, developing and making a brand new drug safely available for any disease normally takes at least 10 years. So, the fastest way to find a treatment for COVID-19 is to identify an existing drug, already approved for some other disease, that is effective against the SARS-CoV-2 virus.
Remdesivir and Dexamethasone are two such drugs that are so far showing the most promise. But it’s unlikely that researchers will find an existing drug that provides a single “magic bullet” for COVID-19. It is more likely that instead a variety of drugs will be identified that can help treat the disease in different ways in different people. Fingers crossed!
Banner: Getty Images