
Health & Medicine
Will COVID-19 change healthcare for stroke patients?

For the first time, researchers show that immune cells help control blood flow, and may hold the key to treating conditions like diabetes, Alzheimer’s disease and stroke
Published 19 December 2021
For around 1.7 million Australians living with diabetes – and the additional 280 people developing the disease every day – new research could form the basis for developing life-changing therapies that limit the impact of diabetic eye disease.
Almost everyone with type 1 diabetes and more than 60 per cent of those with type 2 diabetes will develop some form of diabetic eye disease within 20 years of diagnosis, according to Diabetes Australia.

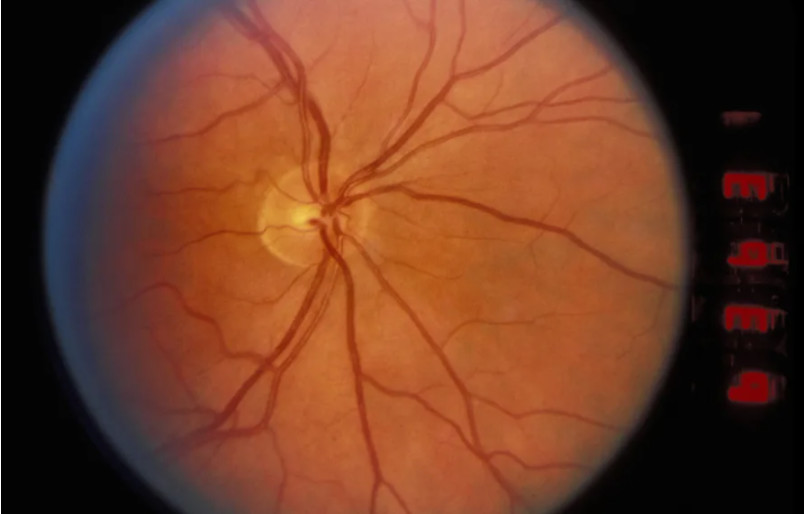
New research, published in the journal PNAS, shows how blood vessels in the back of the eye are regulated, with the results suggesting vascular regulation is more complex than previously thought.

Health & Medicine
Will COVID-19 change healthcare for stroke patients?
University of Melbourne researchers found immune cells – called microglia – make contact with both blood vessels and neurons in the retina and can change blood flow to meet the needs of neurons.
Co-authors, Professor Erica Fletcher and Dr Andrew Jobling identified the chemical signal that immune cells use to communicate with blood vessels and demonstrated that immune cell regulation of blood vessels is abnormal in diabetes – a disease known to affect the blood vessels in the eye.
Importantly, they were able to show that at an early stage of diabetes – before there are any visible changes at the back of the eye – blood vessels are abnormally narrow, affecting the way they supply the neurons of the retina.
Retinal immune cells were implicated in this early vascular abnormality, implicating them as a novel therapeutic target for controlling early changes in the retina in diabetes.
To find out more, we asked the School of Biomedical Sciences researchers about their findings and what needs to happen next to improve the health outcomes for those living with diabetes and other vascular conditions of the retina and brain.
These are highly novel findings, that expand what we know about immune cells in the retina and brain.
Up until only recently, immune cells of the nervous system were thought to sit quietly, only responding when injury or disease occurred. Our finding expands our knowledge of what these cells do and shows a highly unusual mechanism by which blood vessels are regulated.

Health & Medicine
Mapping eye disease
This is the first time that immune cells have been implicated in controlling blood vessels and blood flow.
In the nervous system, vascular regulation has been attributed to a support cell called an astrocyte. Our results suggest that vascular regulation is more complex than previously thought.
Our studies were performed in preclinical animal models that allow us to see retinal immune cells in a living eye.
We used transgenic mice in combination with a range of imaging methods to look at how retinal immune cells communicate with blood vessels.
We also isolated retinal immune cells from groups of normal and diabetic animals and analysed their genome to identify how these cells communicate with blood vessels.
Finally, we used a range of pharmacological tools to examine in great detail how blood vessels change in response to the activation of retinal immune cells.

The major implication of these findings is understanding the abnormal vascular function at an early stage of diabetes.
Diabetes is one of the leading causes of irreversible vision loss, especially in those of working age.

Health & Medicine
Is treating obesity the future of managing type 2 diabetes?
We also know that diabetes can affect all cells in the retina. These results suggest that there are vascular deficits from a very early stage of diabetes that are caused by anomalies in immune cells.
In the longer term, understanding how retinal immune cells change during diabetes may lead to new treatments that can be used from an early stage of disease, well before any loss of vision.
Our results implicate retinal immune cells in the early changes in diabetes, highlighting a new way of controlling and potentially preventing retinal changes in diabetes.
This finding also has implications for our understanding of other diseases of the retina and the brain.
While our study was directed at understanding the function of retinal immune cells in diabetes, a part of it also considered whether the brain’s vascular system is regulated in a similar way. We found that the same signalling mechanism modulates blood vessel function in the brain.
Although only at an early stage, these findings suggest a novel way for understanding vascular diseases of the brain with implications for our knowledge of stroke and Alzheimer’s disease.
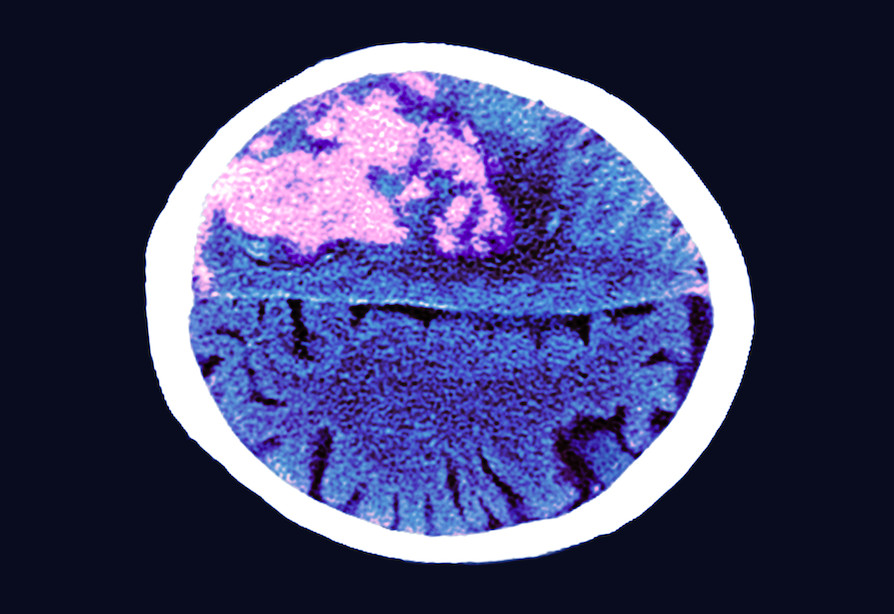
We hope that the findings of this study will form the basis for developing novel therapies for reducing the effects of vascular conditions on the retina and brain.
These conditions include diabetes, Alzheimer’s disease and vascular conditions such as stroke or retinal vascular occlusions.
Banner: Getty Images