Health & Medicine
Reinfection in COVID-19
Last week we looked at a well-documented case of reinfection with SARS-CoV-2. This patient remained asymptomatic following the second experience, which clearly boosted his immunity. But what does it tell us about protective immunity in SARS-CoV-2 infection?
Published 17 September 2020
Last week we looked at a well-documented case of reinfection (see Reinfection in COVID-19 - part one) with SARS-CoV-2. A Hong Kong resident who had COVID-19 and developed some symptoms tested positive again 142 days later when checked by PCR at the airport on his return from a business trip to Europe.
That was not too concerning as he remained asymptomatic following the second experience, which clearly boosted his immunity. But what does it tell us about protective immunity in SARS-CoV-2 infection?

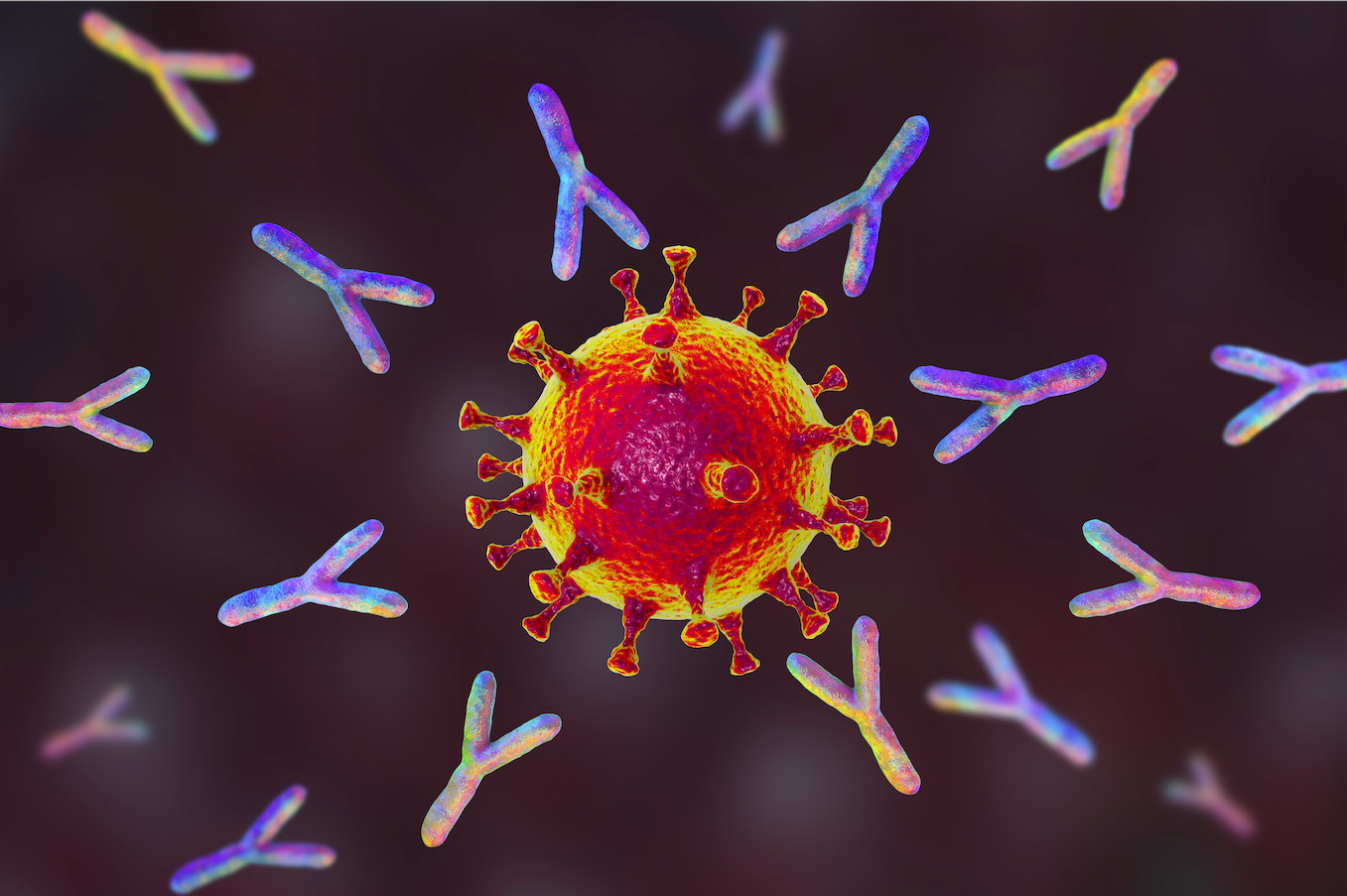
As discussed in previous essays, the primary protection against infection of the nose and mouth regions is the physical barrier of the mucus (slime and snot) layer that bathes the epithelial cells, plus any pathogen-specific IgG and IgA class antibodies that happen to be present.
Health & Medicine
Reinfection in COVID-19
Like virus particles (virions), antibody molecules do not, unless they are bound to a motile cell like a monocyte via their Fc region (the base of the IgG ‘Y’), have any kind of ‘motor’. Both are floating around in the mucus layer without any kind of ‘dating app’ to bring them together.
And the receptor binding domain (RBD) on the SARS-CoV-2 spike protein has a high affinity for (is massively attracted to) the ACE2 molecule that is present on infectible epithelial cells so, in the absence of lots of top quality antibodies in mucus, it’s pretty likely that the virus will bump into an ACE2+ target cell before it’s ‘grabbed’ by the ‘right’ IgG or IgA.
Furthermore, unless a bound Ig molecule or two triggers some virus-destruct mechanism - being eaten by a macrophage or being blown to bits by complement - the Igs would have to block all 30+ spike protein RBDs to prevent any possibility of ACE2 attachment, virus internalisation and replication.
We don’t know how fast the virus grows in the epithelium of the human nose but it’s likely that, within 12 hours or so, a single infected cell could be producing hundreds of infectious virions.
And it seems that SARS-CoV-2 can be passed on by abnormal extended processes called filopods that ‘reach out’ and punch holes in the membranes of adjacent cells.
Health & Medicine
Your protective Igs: The major focus of COVID-19 vaccines
Thus, while any released virus in mucus might be mopped up by an emerging, secondary IgG or IgA response, there may also be localised, multicellular, virus production ‘facilities’ that would resist antibody attack.
We haven’t yet got to the assassins of the immune system, the CD8+ ‘killer’ T lymphocytes, but that’s their job, knocking out these virus ‘factories’.
Under public health surveillance protocols that have operated for virus diagnosis and control until this current pandemic, our Hong Kong patient would not have been tested again for the presence of any pathogen unless he developed fairly obvious symptoms.
A common-cold-like event would likely have been dismissed as just that, meriting no further analysis. With COVID-19 he was, like many asymptomatic people in community surveys, tested in the absence of any obvious disease when he arrived at the airport.
Previously, we’ve only done that by screening for serum antibodies as a measure of past infection. And such antibody assays would not have shown that our Hong Kong subject had been infected with two different virus strains.

We also need to be aware that the PCR test used to determine the presence of SARS-CoV-2 is extremely sensitive, with a capacity to detect around 1000 virions, some of which may not be infectious but still carry the RNA that encodes the SARS-C0V-2 spike protein.
Health & Medicine
Watch Episode 6: Life Beyond Coronavirus: The Expert View
What this tells us is that the positive test for the reinfected Hong Kong subject was definitely finding evidence of a current, or very recent (residual RNA), infection, not just virus in the air that he’d happened to breathe in (he would have been wearing a mask anyway) on the plane or at Hong Kong Airport. And he was OK!
Much more concerning though is a report from the University of Nevada, Reno, School of Medicine, that again used gene sequencing to confirm reinfection. The patient in question tested positive by PCR on 18 April during a community-based surveillance program and became symptomatic a week later, but had apparently recovered by 27 April.
Then, after two negative PCR tests, the patient again sought care on 31 May with (similar to his first set of symptoms) fever, headaches, dizziness, cough, nausea and diarrhea.
Within the week he was hospitalised, requiring oxygen support, and had evidence of lung damage (detected by X-ray) that was not present six days earlier. At this time, his PCR was positive for what looks to be a different SARS-CoV-2 sub-strain.

It’s possible that this clinical recurrence could be a ‘long hauler’ (sporadic, or continued recurrence of symptoms) held over from the first infection. But the change in lung pathology makes it much more likely that the relapse was caused by the new virus.
Next week, we’ll consider the implications of the possibility that reinfection with minimal, or greater, severity may occur in the absence of other, known co-morbidities.
We’ll look at this from the aspect of the ‘long hauler’ phenomenon, and in regard to ideas about herd immunity and the prospects for effective vaccines.
Banner: Getty Images