
Health & Medicine
AI joins the fight against superbugs
Bacteria-killing viruses were used more than 100 years ago to treat infections, and now, as antibiotic-resistant infections increase, researchers are studying how we could bring them back
Published 10 September 2025
Every minute, all around us, battles are fought on a microscopic level.
Bacteriophages (also known as phages) are viruses that infect and kill bacteria. Just like viruses that infect us, these phages seek to steal the resources of the bacteria to replicate and survive.

Phages were independently discovered by Frederick Twort in 1915 and Félix d’Hérelle in 1917.
By the 1920s, d’Hérelle had begun using phages to treat bacterial infections, laying the groundwork for what became known as phage therapy.
However, the discovery of penicillin by Alexander Fleming in 1928 sparked the antibiotic revolution, which soon eclipsed phage therapy and transformed modern medicine, saving millions of lives over the past century.
Now, the rapid rise of antibiotic resistance, also known as antimicrobial resistance (AMR), is threatening to undo past progress.
The World Health Organization (WHO) estimates that antimicrobial resistance could result in up to 10 million deaths each year by 2050.

Health & Medicine
AI joins the fight against superbugs
Other experts warn we may be approaching a post-antibiotic era, where even minor infections could once again become deadly because existing drugs no longer work.
In a new paper published in Cell Reports, our research team based at the University of Melbourne and the Hebrew University of Jerusalem studied how phages interact with bacteria and how bacteria try to fend them off.
Understanding these steps is key to designing effective phage therapies that don’t require antibiotics.
Phages begin their life cycle by attaching to a bacterial cell and injecting their DNA. Once inside, they hijack the bacterium’s cellular machinery to produce copies of themselves.

Eventually, the host cell bursts, releasing new phages that go on to infect other bacteria. Because phages can’t reproduce without a host, this relationship is entirely one-sided, offering no benefit to the bacterium.
Therefore, bacteria have developed an impressive arsenal of defences to survive phage attacks.
One of the most fascinating and well-known defence mechanisms is where bacteria can cleave the phage DNA directly or strip away essential genetic components needed for replication.
Known as the CRISPR-Cas system, the technique operates much like a bacterial immune system.
Health & Medicine
Into the wild to fight antibiotic resistance
Understanding the arms race between phages and bacteria not only deepens our knowledge of how bacteria defend themselves but also opens the door to next-generation treatments.
Our latest work looked at how the bacterial immune system works, finding weaknesses that could be used as targets for phage-based treatments.
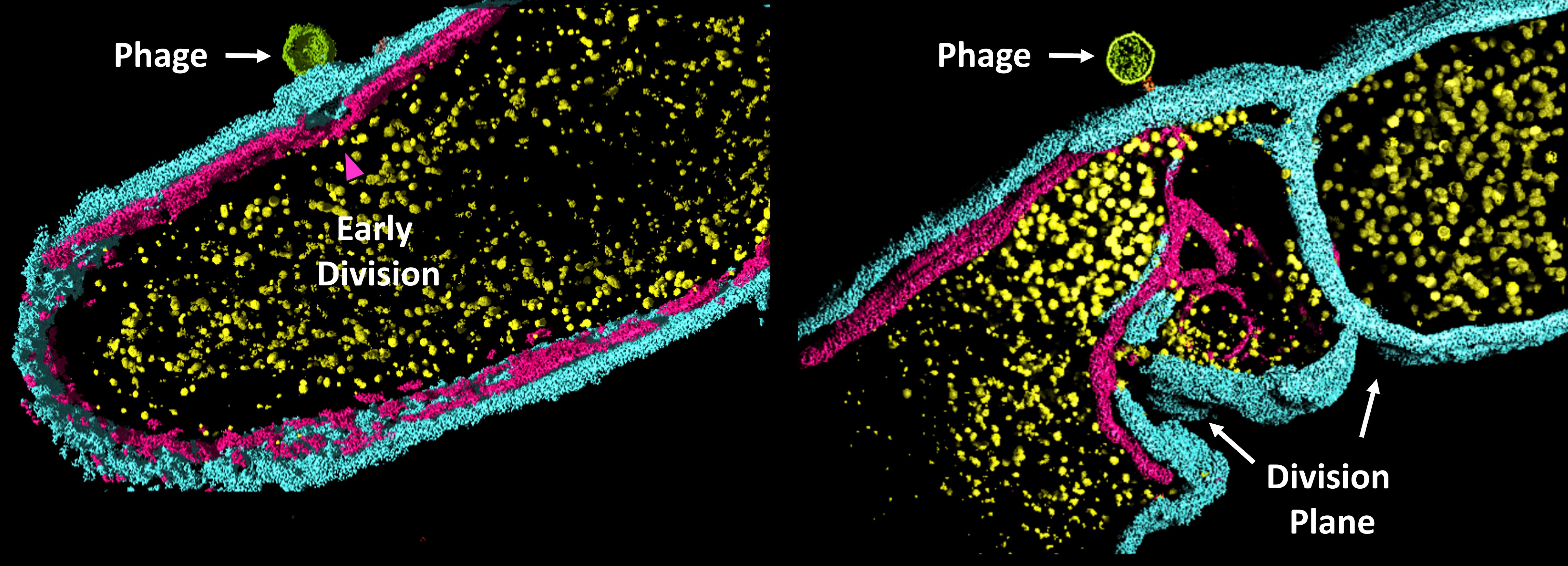
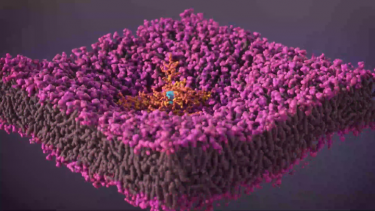
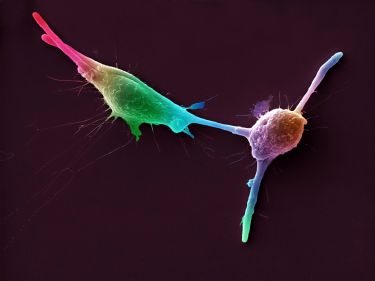
Using advanced bacterial genetics, fluorescence microscopy and high-resolution cryo-electron tomography (imaging in 3D), we identified a bacterial ‘sensor protein’ called YjbH.
Bacteria use this protein to defend against phage attack by preventing the phage from infecting neighbouring bacterial cells.
It works a bit like containing house pests through extreme quarantine.
Imagine if you notice termites in a part of your house, you would want to restrict it immediately before it spreads everywhere. YjbH operates similarly when it detects invading phage DNA and binds to it.
But simply binding isn’t enough; the threat must be contained, or it could replicate and spread throughout the bacterial population, just like a termite spreading through your house.
YjbH rapidly activates cell division machinery by binding to a key cell division protein called FtsE.
This results in constriction of the envelope that surrounds the bacterial cell, which is eventually cut off to isolate the infected part of the cell.
The result is a newly formed compartment that walls off the invading phage DNA.
Health & Medicine
How to SNAPP a bacterial cell
Crucially, this isolated compartment lacks the resources needed for the virus to replicate, effectively trapping the infection and allowing the rest of the bacterial cell to survive.
These observations suggest that bacteria, despite being single-celled organisms, are capable of a dramatic escape strategy similar to those seen in higher organisms.
Just as doctors may amputate an infected limb to save a life, or lizards shed their tails to evade predators, these results show that bacteria can isolate and sacrifice an infected part of themselves to survive a viral attack.

This phenomenon, similar to ‘bacterial autotomy’, marks the first discovery of such an anti-phage defence system.
It reveals that even microbes can perform complex, self-preserving escape responses, once thought to be exclusive to multicellular life.
Now that this defence mechanism has been identified, our next step is to develop different ways to neutralise it.
These could include creating a compound that can be added to the phage therapy, preventing the sensor protein from identifying different phages.
Health & Medicine
Why antibiotics give you thrush and other microbiome mishaps
We hope that by reactivating phage therapy, we can contribute to non-antibiotic treatments for infections.
With so many antibiotic-resistant infections emerging, after 100 years, it’s time to reconsider the benefits of phage therapy.
The research project was co-led by Associate Professor Debnath Ghosal from the University of Melbourne and Professor Sigal Ben-Yehuda from the Hebrew University of Jerusalem, and included PhD student Somavally Pundalik Dalvi.