Health & Medicine
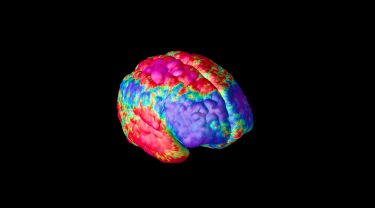
Mapping how schizophrenia changes brains

A new brain scanning technique reveals how changes in white and grey matter seen in schizophrenia are linked, and how the brain compensates for these changes, at least in the illness’s early stages
Published 18 November 2018
Over the last two decades, research has started to reveal the details of what’s happening in the brains of people with schizophrenia.
Thanks to new brain imaging techniques we can now see the many changes taking place when someone has this devastating illness.

In particular, the symptoms of schizophrenia, like hallucinations, delusions and difficulty thinking, have been linked to a breakdown in communication across the brain.
Connecting how these changes relate to each other is an important step in understanding how schizophrenia progresses. Ultimately it may help us find treatments that change the course of these brain changes, and reduce or eliminate symptoms.
Health & Medicine
Mapping how schizophrenia changes brains
While researchers have previously observed changes in the brain’s two types of tissues – grey matter and white matter – few human studies have explored whether these two factors are related or separate disease processes.
In research published in Schizophrenia Bulletin we looked at brain images of 200 schizophrenia patients (and 150 healthy controls) and found that disruptions in the brain’s white matter are intimately linked to changes in grey matter regions in the cerebral cortex.
We also found that these changes tend to evolve together throughout the course of illness, and that, surprisingly, the brain compensates for some of the damage caused – at least in the early stages.
White matter in the brain is responsible for transmitting electrical signals that brain cells use to communicate. These signals are transmitted along axons (nerve fibres), which are insulated by a fatty substance called myelin.

Subtle changes in this wiring have been found in the brains of people with schizophrenia. For example, changes in the thickness and structure of myelin can influence the timing and velocity of brain signals, leading to some of the cognitive difficulties patients experience.
Loss of grey matter density in the cerebral cortex is also seen in people with this illness. Grey matter comprises the cell bodies of nerve cells, and its density has been linked with abilities like academic and musical performance.
Health & Medicine
Brain ever changing: Neuroplasticity and its role in mental health
Interactions between grey and white matter have been found at a cellular level.
We used magnetic resonance imaging (MRI) technology to take detailed pictures of each subject’s brain, collecting two image contrasts – one that was sensitive to overall brain structure (especially grey matter) and another that captured the organisation of white matter.
We developed a new imaging technique to map the brain, which could jointly image grey matter and white matter, to examine whether the changes that we see in both tissue types are linked. We did this by capturing grey matter and directly adjacent white matter across multiple depths in the brain.
Conventional imaging methods typically address one aspect of disease (or pathological process). But our ability to map across tissue types opens new avenues for testing how multiple aspects of the disease are interacting in the brain.
By mapping the brain’s white and grey matter in a large population of schizophrenia patients, we demonstrated that the changes we see in grey and white matter are in fact related processes in schizophrenia, and that this relationship evolves as the illness progresses.

With younger patients, the most marked alterations are lower levels of grey matter in the frontal regions of the brain. These frontal grey matter regions are initially surrounded by relatively strong white matter connections. However, there is a noticeable turn in older patients. As the illness progresses, the strength of frontal white matter connections rapidly weakens.
We see this manifest in cognitive impairments in young people, which becomes more pronounced in older patients.

Health & Medicine
Can sunshine help your brain?
This white matter decline transforms the overall pattern of brain abnormalities in older patients with schizophrenia, whereby compromised levels are eventually discernible in both grey and white matter structures and span many regions across the brain.
Taken together, these findings show that grey and white matter changes don’t occur in isolation, but rather interact to produce complex patterns of brain change across the course of illness.
While we saw extensive loss of grey matter in our subjects, which is consistent with previous imaging studies, surprisingly we found that white matter was enhanced in the areas with the most extensive grey matter loss.
This suggests that white matter may be compensating for grey matter loss, at least in the early stages of the illness. These findings could point to an extremely flexible compensation strategy in the brain, with stronger white matter connections strengthening communication to compromised grey matter.
However, it is likely this compensation is costly and unsustainable in the long term. With progression of the illness and grey matter loss over time, further brain alterations could lead to the pattern of widespread alterations in both tissues that we see in patients with prolonged or chronic schizophrenia.
Ultimately, this study underscores a need to move beyond investigating the impacts of this disease, and others, in isolation, and instead, connect the dots by testing interactions between different disease processes.
Unveiling these linkages will help us understand the disease in much more detail, and ultimately help us better treat people with schizophrenia.
This research was conducted by researchers from the University of Melbourne, Monash University, the University of Sydney and the QIMR Berghofer Medical Research Institute.
Banner image: Getty Images