Health & Medicine
New immune cells help maintain breast health

Researchers have developed a modified form of human insulin that successfully mimics the ultra fast-acting properties of cone snail venom insulin
Published 5 June 2020
Underneath the intricate patterns of the cone snail’s shell hides a collection of chemicals that are providing a ‘blueprint’ for new medicines.
Moving slowly across the sand on a muscular foot, the cone snail needs fast-acting venom that immediately paralyses small fish before they can swim away.

So far, around 700 cone snails, or Conus species have been identified in tropical and sub-tropical regions around the world, and each possess an average of 100 to 200 conotoxins.
This ‘cocktail’ of toxins targets the skeletal and heart muscles, as well as the central nervous system, but it also lowers blood sugar to reduce mobility and consciousness, providing many valuable lessons for drug discovery.
Health & Medicine
New immune cells help maintain breast health
In the hope of improving diabetes treatment, Melbourne scientists are focusing on the blood sugar function of the venom.
By creating a modified form of human insulin, they have successfully incorporated the ultra fast-acting properties of cone snail venom insulin from the species Conus geographus.
The research is a collaboration between the Walter and Eliza Hall Institute of Medical Research (WEHI) and the University of Utah, along with researchers from the University of Melbourne, La Trobe University, Flinders University and Monash Institute of Pharmaceutical Sciences.
Professor Mike Lawrence, WEHI’s lead researcher on the study, has been investigating the structure of insulins and their function for almost two decades.
“Essentially, we wanted to take the fast-acting nature of the snail venom and combine it with the therapeutic properties of human insulin,” Professor Lawrence says.
He explains that “the problem with human insulin is that it needs to aggregate to be stored in the pancreas. These aggregates must break up into individual molecules before they can begin to work on blood sugar, a process that can take up to an hour when insulin is used by diabetic patients.”

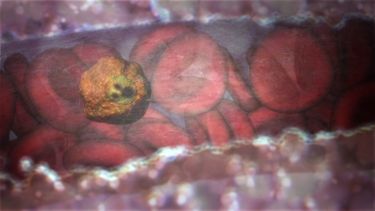
The hormone, insulin, is normally released rapidly from the pancreas after a meal, when the level of blood sugar — glucose — is high.
The hormone works by stimulating the uptake of glucose into cells; muscles can take up glucose to use for immediate energy or it can be stored in the liver as glycogen until needed. Diabetes occurs when your body doesn’t use insulin properly or doesn’t make enough insulin, so injections of the hormone are needed to help manage glucose levels.
Health & Medicine
Exposing malaria’s atomic machinery
“Our ultimate aim is to help people with diabetes to control their blood sugar more tightly and rapidly,” Professor Lawrence says.
“Faster-acting insulin may help diminish the risk of hyperglycemia [high blood sugar] and other serious complications of diabetes. It also could improve the performance of insulin pumps or artificial pancreas devices, which automatically release insulin into the body as needed.”
Working closely with Professor Lawrence at the Walter and Eliza Hall Institute is Dr John Menting.
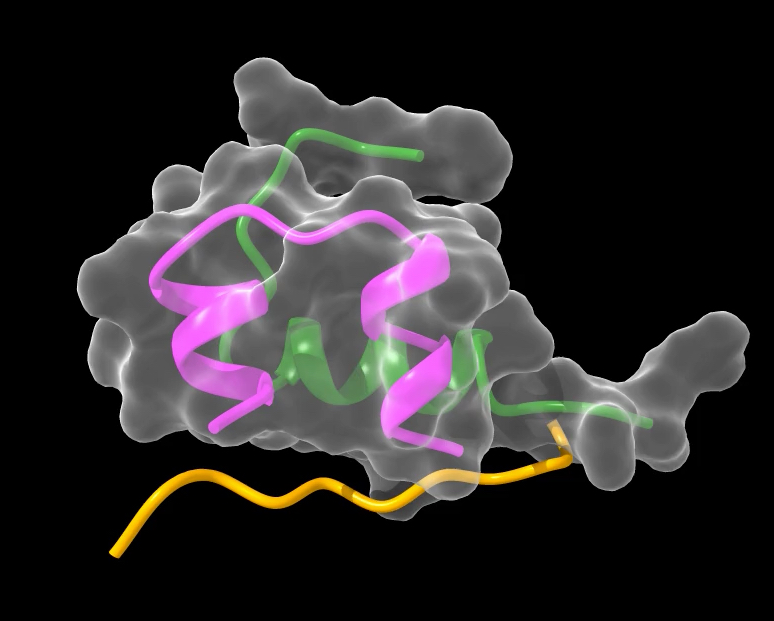
“Just like any engineering project, our study required detailed images of the cone snail insulin to know which ‘design changes’ could be made to improve the effectiveness of human insulin,” Dr Menting says.
Working with the Australian Synchrotron, the team studied the structure of the cone snail insulin in molecular detail, finding that it had the same basic structure as human insulin but lacked the ‘hinge’ component that causes aggregation.
But although it is faster acting, the cone snail’s insulin is far less potent than human insulin and would not be useful in itself as a therapeutic.
It would also likely be immunotoxic, which can damage the immune system by destroying immune cells and changing signalling pathways.
“So our team identified four amino acids [protein building blocks] that help the snail venom insulin bind to the insulin receptor,” Dr Menting says. “We then began by creating a shortened version of a human insulin molecule without the region responsible for its aggregation.”
Sciences & Technology
Magnetic teeth revealed using quantum imaging
“The modified versions of the cone snail amino acids were then integrated into the human insulin molecule with the goal of creating a hybrid that would bind the human insulin receptor with high potency and without the capacity for aggregation.
“We call the new hybrid insulin ‘Mini-Ins’, short for mini insulin.”
In tests with animal models, the hybrid insulin molecule was found to lower blood sugar rapidly levels after meals.
“We have completed the translational step from a cone snail venom insulin to a human look-alike, Mini-Ins, that is safe and well-tolerated by the immune system, a vital consideration when developing new diabetes treatments,” Professor Lawrence says.
“Our findings also showed that Mini-Ins doesn’t activate the related insulin-like growth factor pathways that would increase the risk of cancer – something researchers need to absolutely avoid when developing new insulin treatments for diabetes.
“Even at this early stage of development, Mini-Ins was able in animal models to lower blood sugar levels as fast as the current best treatments that are in use. This tells us that with further development, the response time could be made even shorter. For diabetes patients this could be life-changing.”

According to the World Health Organization, diabetes impacts more than 422 million people worldwide. For many people living with diabetes, it can be challenging to consistently manage blood sugar levels by injecting insulin well before having a meal.
As a consequence, there is often a lack of compliance with the injection regime that then has negative health consequences, says Professor Lawrence.

Health & Medicine
Science, society and drug design
“Our goal is to improve insulin treatments by shortening the timeframe it takes for them to work. Achieving this would help people with diabetes to more easily manage their condition which would in turn lead to better health outcomes,” he says.
The researchers are now working with a commercial partner to progress the Mini-Ins proof-of-concept towards the development of a therapeutic version that is safe and effective in humans.
“These are exciting next steps. Our goal is that a future version of Mini-Ins could end up being used by patients around the world,” Professor Lawrence says.
“The aim of this next phase is to progress treatment to clinical trials and hopefully, one day, achieve a safe and effective insulin treatment that works faster than the current gold standard. Even being able to halve the pre-injection timeframe would make a huge difference for people living with diabetes,” he says.
The research was supported in Australia by the National Health and Medical Research Council. It was supported in the USA by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and the JDRF.
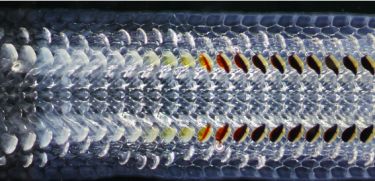
Banner: Textile cone snail: Shutterstock