
Health & Medicine
Is treating obesity the future of managing type 2 diabetes?
For the first time, research has shown that impaired brain cells linked to body weight and hunger can be restored - opening up new treatments for obesity and type 2 diabetes
Published 19 September 2024
Diseases involving our metabolism – including obesity and type 2 diabetes – affect more than a quarter of the global population and are projected to become the leading cause of death by 2030.
With no effective long-term treatments currently available, their prevalence is expected to cost Australian's $AU87.7 billion per year by 2032.

The quest for effective treatments for obesity and type 2 diabetes has now been identified as a paramount global health imperative, presenting one of the most important clinical challenges of our lifetime.
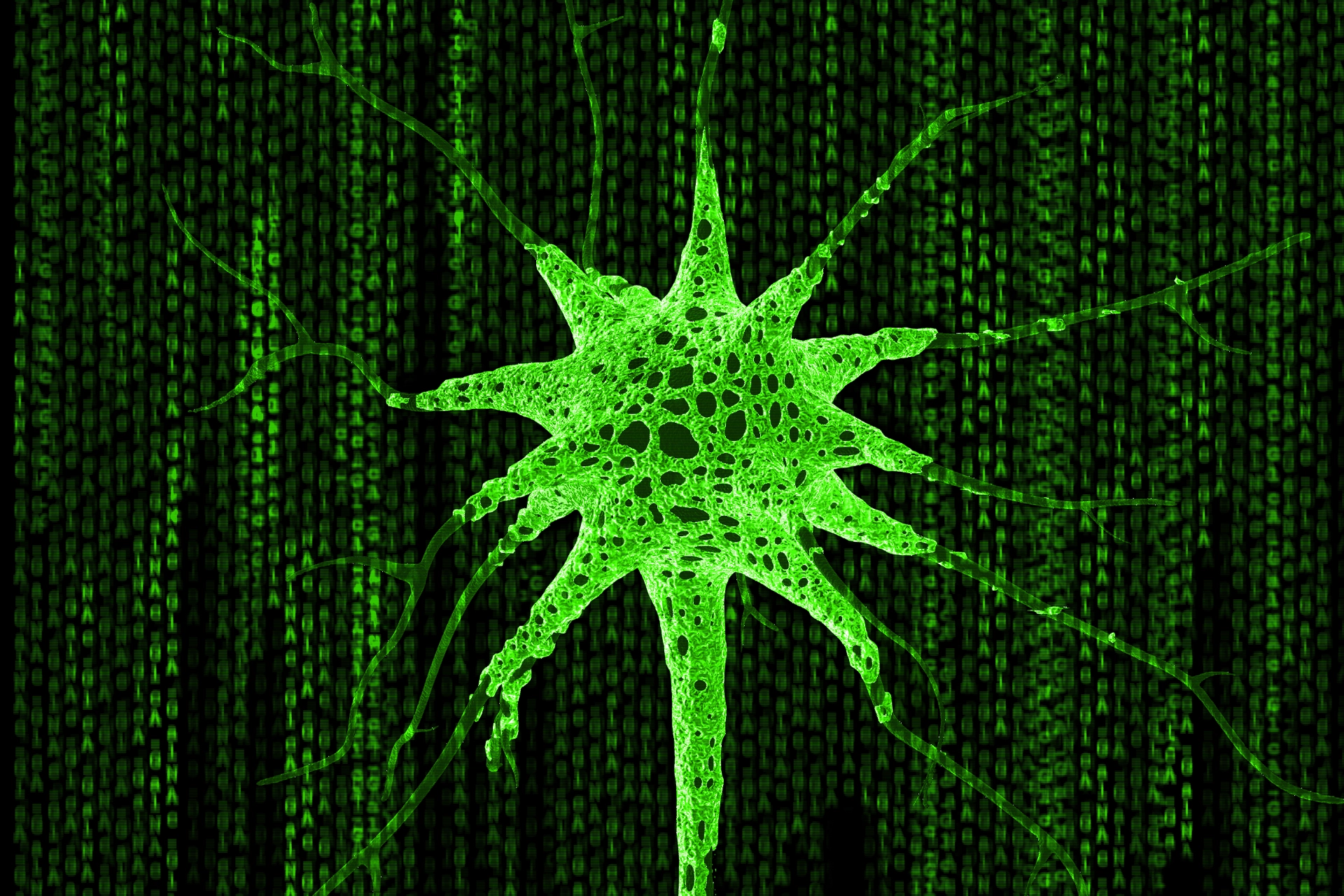
Our latest research, published in Nature, focuses the discovery that our brain cells (neurons) can become trapped in a dense, glue-like substance known as the extracellular matrix (ECM) when a person is obese or has type 2 diabetes.
We have called this condition neurofibrosis because the brain cells effectively become thickened, like scar tissue.
Using animal models, we found that when these neurons are encapsulated in the matrix, it prevents them from functioning properly, affecting their ability to control body weight, hunger and blood sugar levels.

Health & Medicine
Is treating obesity the future of managing type 2 diabetes?
Until now, the neurofibrosis process was considered irreversible.
But, for the first time, our precise targeting research has shown that the function of these cells can be restored – providing new possibilities for the treatment of obesity and type 2 diabetes.
While we know a lot about the different cell types in our bodies, like bone and muscle, the significance of the spaces between these cells – known as the extracellular environment – is often overlooked.
This environment, which varies across cell types, tissues and health states, is crucial for cell communication and function.
A key component of this extracellular space is the ECM, a complex network of sugars and proteins. The ECM not only provides structural support but also plays a vital role in regulating how our cells interact.

In conditions like obesity and diabetes, we know that the ECM around liver and fat cells becomes thicker and dysfunctional. This process is called fibrosis and is usually irreversible.
Our research focuses on a similar thickening of the ECM around neurons that govern our appetite, body weight and glucose regulation.
This thickening, or neurofibrosis, leads to impaired function of these critical brain cells as diseases like obesity and diabetes progress.
One of the main ways our body regulates blood sugar is to secrete the hormone insulin from the pancreas, moving sugar out of the blood into our muscles and liver.

Health & Medicine
Could your GP prescribe a Parkrun instead of a pill?
But in conditions like obesity and type 2 diabetes, neurons in the brain develop insulin resistance – impairing their ability to regulate blood sugar levels and appetite effectively.
And this can then lead to organ damage and heart issues.
We studied the neural circuits at cellular and molecular level in obese and insulin-resistant mice.
This technology is crucial for unravelling the mechanisms of brain dysfunction in human metabolic diseases because rodents develop metabolic diseases in ways remarkably similar to humans.

Our team developed 'first-in-class' neurofibrosis inhibitors that target the extracellular matrix in the brain.
And we discovered that they could restore insulin signalling and overcome insulin resistance.
There are currently no effective therapeutics for alleviating neuronal insulin resistance. So our inhibitors represent a significant advance in treating this core underlying feature of metabolic disease.
They open up a new therapeutic avenue by targeting novel disease mechanisms and addressing previously untreatable aspects of the disease.

Health & Medicine
Personalising blood sugar targets
While the underlying reasons for neuronal insulin resistance and potential reversal methods remain unclear, our study shows that neurofibrosis is a causal factor in insulin resistance.
Our results pinpoint potential new drug treatments that specifically target the extracellular matrix surrounding the brain cells that can cause weight gain and elevated blood glucose levels.
The inhibitors prevent further accumulation of the ECM, which leads to the breakdown of the scar-like ECM.
Looking forward, our research will now focus on understanding how neurofibrosis develops in the brain and also what happens as obesity and diabetes progresses to cause it.

Our ultimate goal is to develop novel neurofibrosis inhibitors, making them available for clinical use within the next three to five years.
We urgently need a ‘win’ in our ongoing battle against these twin global public health concerns.
And our research is a step in the right direction.
Our research team includes Associate Professor Garron Dodd as senior author and Cait Beddows as first author, as well as Feiyue Shi, Anna Horton, Ellie Cho, Magdalene K Montgomery, Matthew Watt, Benjamin L Parker, Robyn Brown (University of Melbourne), Sagar Dalal, Nicolle H Packer, Edward SX Moh (Macquarie University), Ping Zhang, Chang-Chun Ling, V Wee Yong (University of Calgary), Kim Loh (St Vincent’s Institute of Medical Research), and Adam J Rose (Monash University).