Health & Medicine
Caught! The cell behind a lung cancer

New discovery in stem cell bowel cancer research targets dormant cancer cells before they start to grow cancers
Published 25 September 2015
A key to controlling stem cell behaviour that is responsible for the spread of bowel cancer has been discovered by an international team led by University of Melbourne researchers.
Frizzled7, one of the Wnt cell surface receptors, has been identified as the key to stem cell activity that causes cancer to spread.
These findings will help to arrest cancers in patients by targeting both growing and also dormant cancer cells, and will be a major advance from conventional therapies and treatments which primarily target only growing cancer cells.
This innovative approach will be particularly significant for bowel cancer patients. Professor Elizabeth Vincan said:
Health & Medicine
Caught! The cell behind a lung cancer
“The problem with bowel cancer is that when a patient comes for treatment, the cancer is usually advanced and will already have spread to other parts of the body. It can sit dormant for years before starting new cancer growth,’’ says Professor Elizabeth Vincan, from the University of Melbourne’s Department of Anatomy and Neuroscience.
“What we found was if you knocked out Frizzled7 while the cells were in a dormant state they weren’t able to restart the tumour growth. The aim is to try to get those cells while they are sitting there and not growing.
“We knew from previous research that a bowel stem cell, which can be uniquely identified by a cell protein known as Lgr5, is involved in initiating cancer growth. We also knew that that Lgr5 stem cells need proteins such as Wnt, but the exact cell surface Frizzled receptor that binds Wnt was not known.
“There are ten Frizzled receptors and our research revealed that Frizzled7 is the one that is important in Lgr5 stem cells and is the one to target in cancer,” Professor Vincan said.
Stem cells are kept active by Wnt signalling pathways to renew and repair damage in our tissues. In the ideal, they renew exactly the right amount of tissue, however if they are overactive and make too much tissue, cancer will form.
“You can see cancers as parasites, because they use the mechanisms that normal stem cells use,” says collaborator Professor Hans Clevers.
“Cancers take on all the attributes of a normal stem cell, but they don’t know the restrictions of a normal stem cell - how to make just the right amount of tissue and stop when that’s done.”
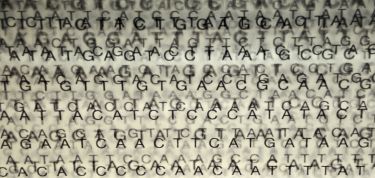
Health & Medicine
A chip off the DNA block
Bowel cancer is the second most common cancer in Australia and is responsible for 80 deaths from cancer each week (Cancer Council of Australia). Globally there were 1.4 million new cases and 694,000 deaths from bowel cancer in 2012 alone (World Health Organization).
“Most people don’t die of primary bowel cancer. Conventional therapies and treatments have poor outcomes for bowel cancer patients because by the time they are diagnosed, the cancer cells have spread to secondary organs and can sit there, undetected, until something triggers them to form a cancer again, and that is what people die of,” Professor Vincan said.
“The next piece of the puzzle is how to target Frizzled7 and develop anti-Frizzled7 antibody treatments that can be used in combination with other current therapies. We are collaborating with scientists internationally who are currently trialling imminent antibody treatments, which will benefit patients with a range of cancers including bowel cancer.
“It represents a shift in the targeted management of cancers.”
These findings are published in the journal Stem Cell Reports.