Health & Medicine
Filling in the genetic blanks of breast cancer predisposition

A new discovery will help doctors deliver more targeted treatments for patients with this devastating cancer
Published 28 September 2018
Ovarian cancer is a scary disease.
Hard to detect, it often isn’t diagnosed until an advanced stage, leading to a five year survival rate of just 43 per cent (by comparison the breast cancer rate is 90 per cent).

And, like many other cancers, research is revealing it is not a simple single disease, but actually multiple diseases driven by a range of molecular differences.
Arming doctors with more precise treatment options is part of the answer, so that they can have a ‘checklist’ of options to match the right treatment to each individual patient.
Health & Medicine
Filling in the genetic blanks of breast cancer predisposition
But now a discovery by researchers at the Walter and Eliza Hall Institute and the University of Melbourne, published in Nature Communications, will help add to this checklist - by revealing differences within a group of patients who previously received the same treatment.
Mutations in the BRCA1 gene predispose patients to developing ovarian and breast cancer at younger ages than the general population; Hollywood actress Angelina Jolie famously had a double mastectomy and surgery to remove her ovaries and fallopian tubes after discovering she carried the BRCA1 gene.
These superstar genes are responsible for repairing damaged DNA but when they mutate, the DNA may not be repaired properly which can lead to cancer developing.
For ovarian cancer patients with this ‘faulty DNA repair’, a group of drugs called PARP inhibitors have been shown to be effective; but not for everyone.
“This drug has been around for over 10 years now and it has been a very exciting development because it’s the first targeted drug used in ovarian cancer and has shown a lot of promise in patients with ‘faulty DNA repair’,” says Dr Olga Kondrashova, one of the lead researchers on the study.
“But we wanted to understand why it wasn’t effective for all patients with BRCA1 methylation, a molecular equivalent of BRCA1 mutation.
“Methylation is molecular silencing, or the ‘switching off’ of the gene.”
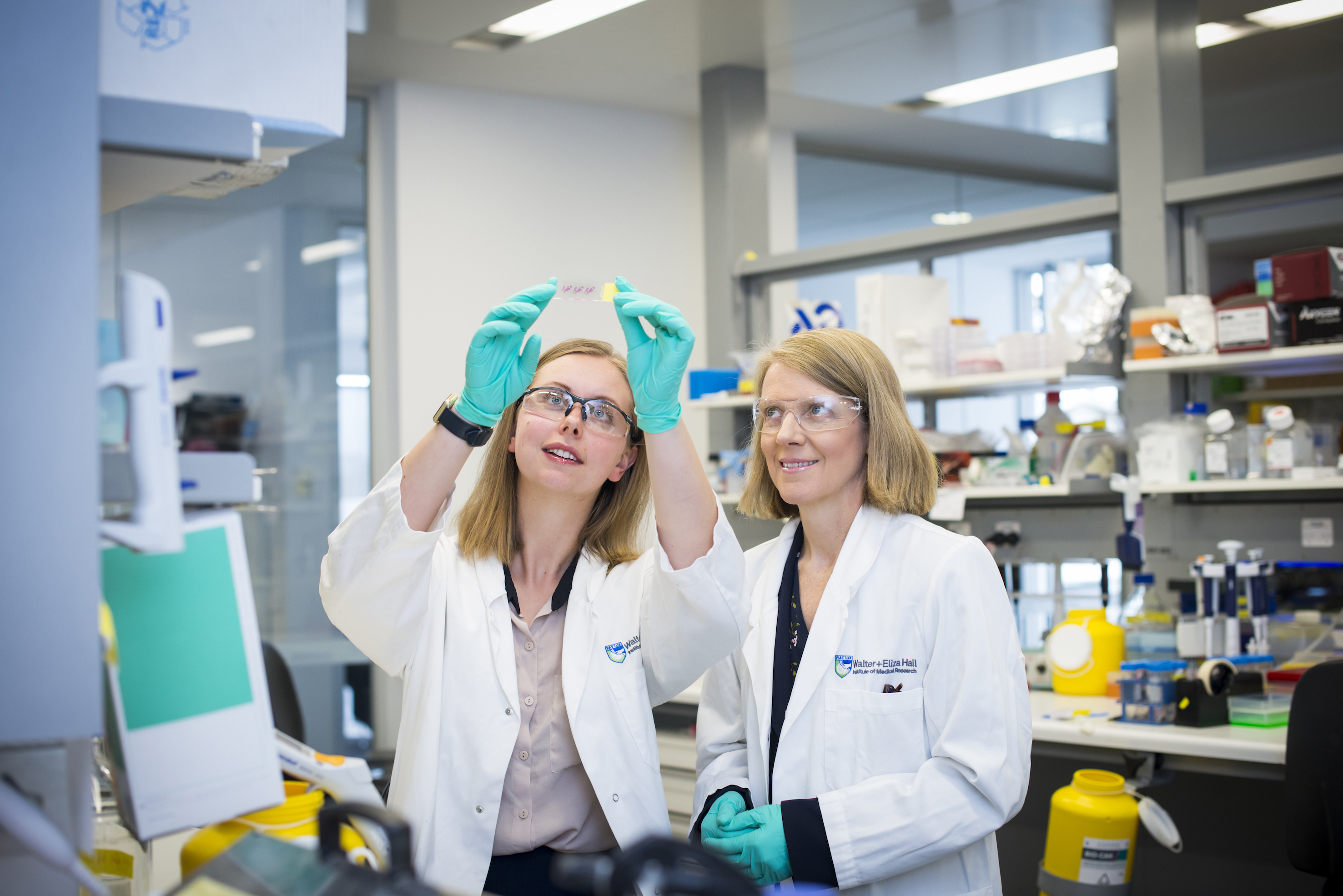
Dr Kondrashova was part of Professor Clare Scott’s research team, which looked in great detail at a small number of samples from patients at the Royal Women’s Hospital in Melbourne, the Royal Melbourne Hospital and the Peter MacCallum Cancer Centre.

Health & Medicine
Busting the myth that endometriosis is a ‘skinny woman’s’ disease
“Rather than studying a lot of patients, we studied a few in great detail,” she says.
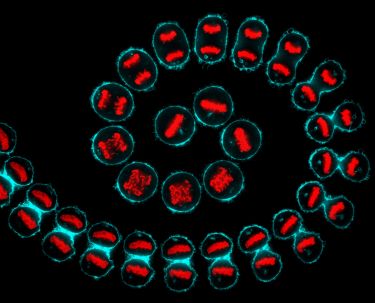
Using patient-derived xenograft models, which are surgical samples that have been refined so they are pure cancer cells, the team was able to separate the patients into two groups after observing differences in their epigenetics.
They found one group of patients had methylation on all copies of BRCA1 genes in their cancer, which meant the gene had been completely switched off. The other group only had partial methylation, which meant the gene hadn’t been totally switched off. So, the DNA repair pathway was not faulty, and the drug was ineffective.
“If you’re just looking at a surgical sample, which most previous studies have done, the normal cells can mask the methylation signals.
“But in our models, we could look purely at the cancer cells, which allowed us to observe these two separate states of methylation.”
Dr Kondrashova says these patients should be considered as two separate groups in light of her team’s discoveries, rather than as the one group they were previously considered.

The researchers have a suspicion that in the patients with incomplete methylation, who don’t respond to the drug, the cancer may have become resistant in response to chemotherapy.
“We think they might have actually had complete methylation, with the BRCA1 gene switched off, at an earlier stage of the disease, but that has changed in response to chemotherapy, which is always the first course of treatment” she says.
“We’re looking into designing a clinical trial that will be done earlier in the disease, ideally before this resistance has developed, to test if this is the case.”
Health & Medicine
Putting cancer cells to sleep
Their findings also show promise for breast cancer treatments, for those patients with BRCA1 methylation.
“In our study we were only looking at ovarian cancer but in principle it could also be applied to breast cancer as well, where BRCA1 methylation is also seen,” says Dr Kondrashova.
The next step for Professor Scott’s team is to investigate more options for personalised treatments for ovarian cancer, just like their colleagues in other areas of cancer research.
“We’re really interested in using combination treatments,” says Dr Kondrashova. “We are involved in a clinical trial looking at combining a PARP inhibitor, with immunotherapy, where the body’s immune system can be reprogrammed to attack the cancer.”
And while chemotherapy is likely to remain the first treatment for ovarian cancer for some time yet, ultimately, the goal is to develop more personalised treatments that can be used earlier in the disease.
“It can take time for research discoveries to translate into clinical setting,” says Dr Kondrashova. “But our research adds to a lot of exciting discoveries in ovarian cancer, and I would hope to see improvements in its survival rates in the not-too-distant future.”
Banner image: Getty Images