Health & Medicine
Enlisting nanoparticles in the fight against superbugs
Chemically altering old antibiotics once thought too toxic for humans is opening a new front in the fight against antibiotic resistance that is now a global crisis
Published 20 March 2018
Tony Velkov remembers his first encounter with antibiotics. He was seven, and it’s fair to say it scarred him for life.
“I’m there seeing the doctor with what was probably just a cold, and he gets out this 22-23 gauge, 1.5 inches long needle and injects antibiotics into my butt cheek. That day sure did create some memories for me,” says the now Associate Professor Velkov, his eyes wide as he relives it.

“The doctor couldn’t have had any evidence that I had a bacterial infection. It could have been a virus. But back then antibiotics were seen as a cure all and he was just giving shots to everyone prophylactically.”
That childhood encounter with a big needle has now come full circle. The University of Melbourne medical researcher is leading work into developing new antibiotics to stay ahead of deadly bacteria that, because of the over-use he was on the wrong end of as a child, are rapidly building resistance.
“Antibiotics aren’t Tic-Tacs, but that is how we have been treating them. We’ve been popping them and now we are in this mess” says Associate Professor Velkov.
Health & Medicine
Enlisting nanoparticles in the fight against superbugs
In 2014, then US President Barack Obama made combating antibacterial resistance a national security priority and the World Health Organization (WHO) has warned that the drug pipeline is inadequate to head off rising resistance in tuberculosis and ‘gram-negative’ bacteria (superbugs that can cause deadly infections in wounds, the lungs, in the blood stream and the urinary tract).
Last year WHO Director-General Dr Tedros Adhanom Ghebreyesus warned that without increased funding for antibiotics research and development “we will be forced back to a time when people feared common infections and risked their lives from minor surgery”.
It is a crisis that has sent scientists scouring the planet for new antibiotic compounds that haven’t been contaminated by human development, and therefore exposed to our bacterial enemies. At the same time researchers like Associate Professor Velkov are going back into the archives to retrieve old antibiotics that were too toxic to have ever been used, to see if they can be chemically altered for human use.
It is, he says, a form of chemical warfare in which he and his colleagues are using intuition built over decades to tweak the chemical structure of antibiotics just enough to make them safe without undoing their killing power against bacteria. And he’s found a particularly ruthless killer in an antibiotic called octapeptin.

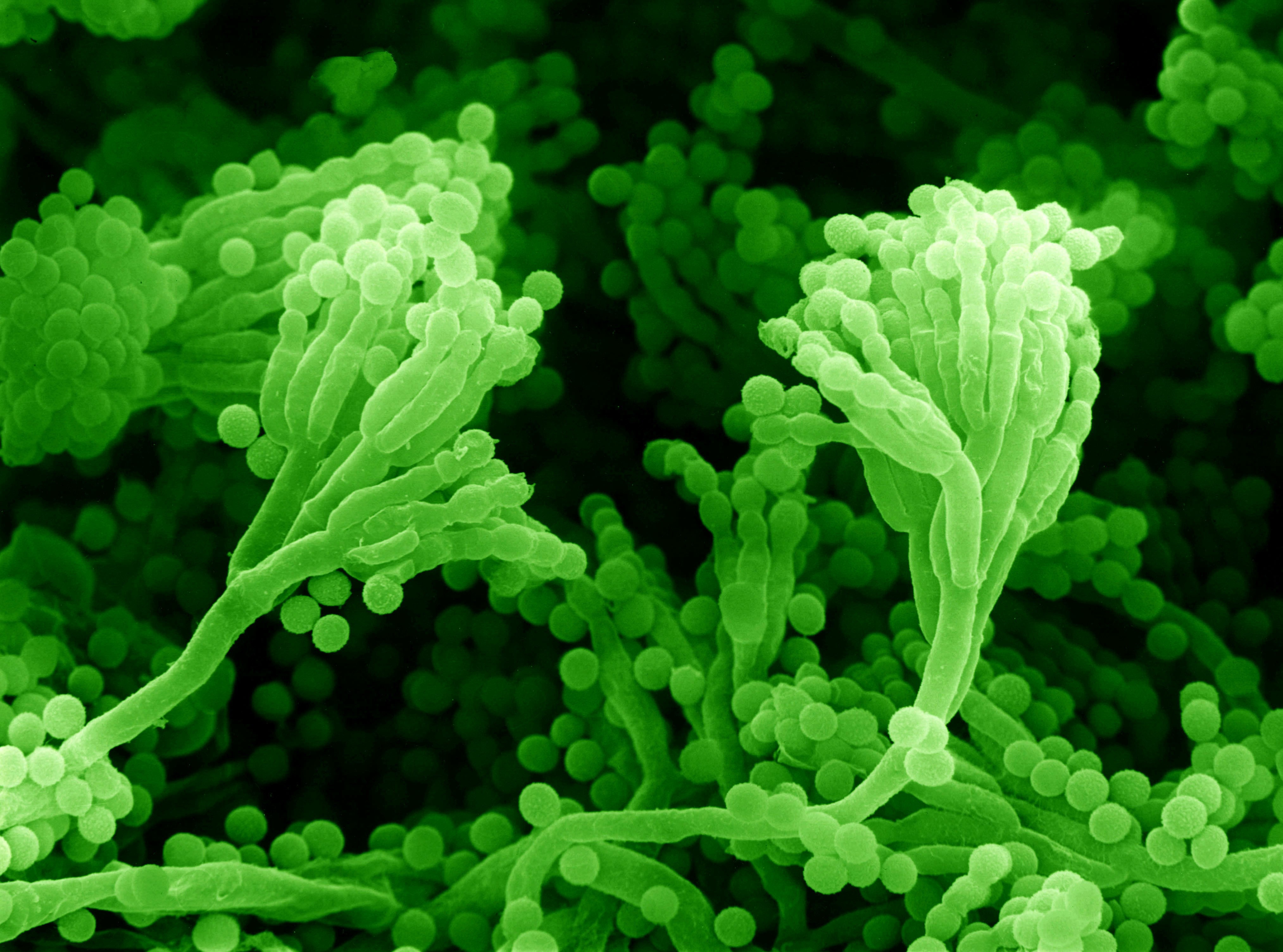
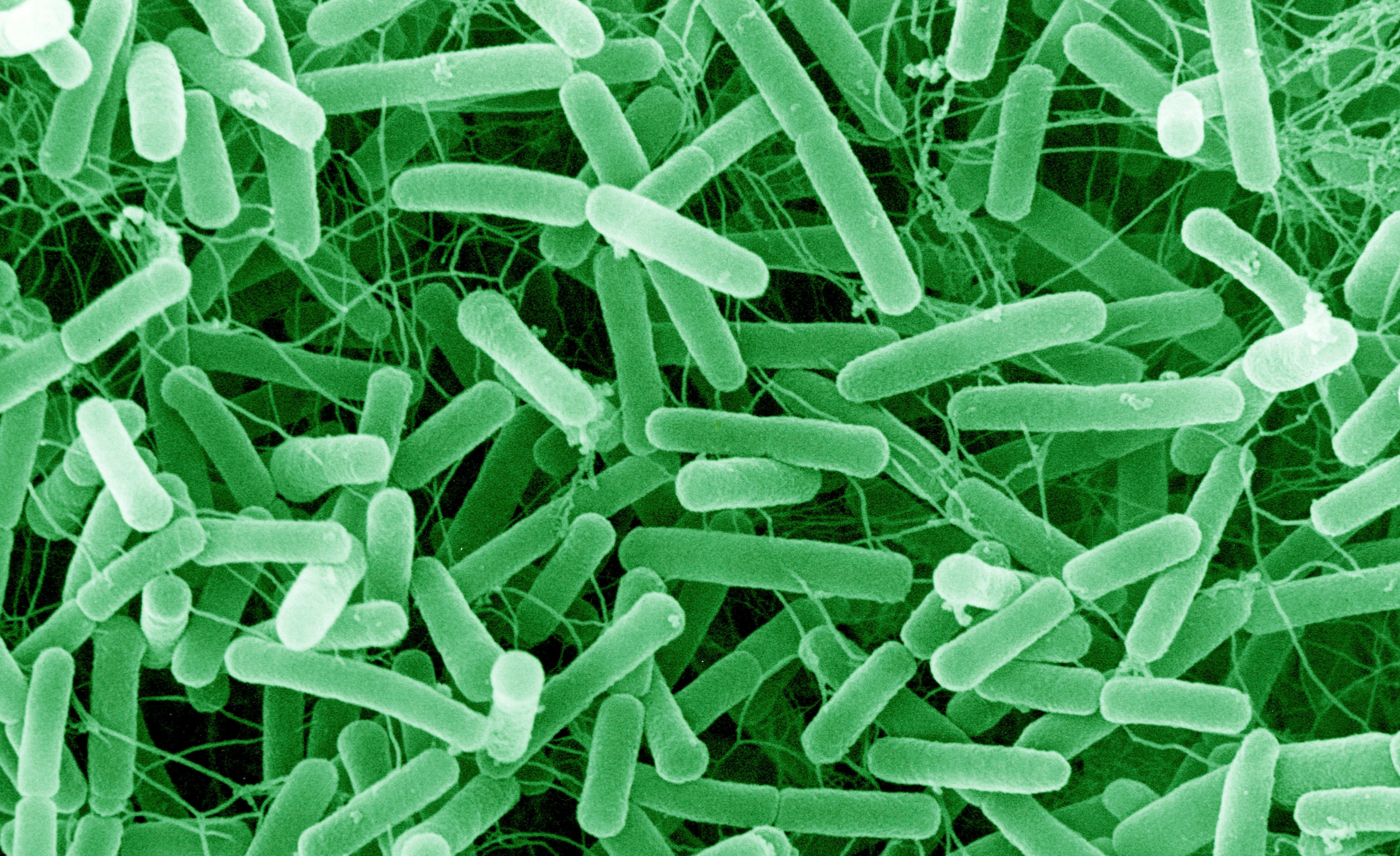
First discovered in soil bacteria in the 1950s, octapeptin has the potential to become a new antibiotic that can kill the very sort of gram-negative bacteria that WHO have said are a research priority.
“With the tools of modern chemistry and biology we are revisiting the old forgotten antibiotics that were left on the shelf as just too hard. And we are finding that in a world facing antibiotic resistance, they can be really important,” says Associate Professor Velkov.
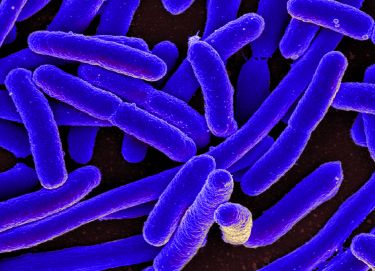
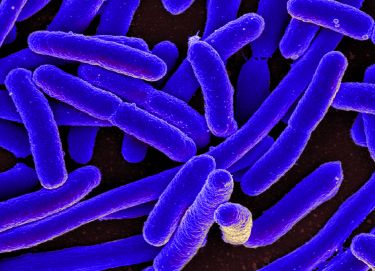
Antibiotics are lethal chemical compounds that are naturally developed by bacteria to eliminate rivals in the unending microscopic war over feeding grounds. Gram-negative bacteria are particularly hardy bacteria because they have an additional cell wall protecting them.
“Ever since the discovery of penicillin in 1928, the first antibiotic, we’ve been exploiting this chemical warfare by using the bug’s chemicals against them.”
Octapeptins, he says, are expert gram-negative bacteria killers. “They just punch holes through them,” he says. “They are like a sledge hammer to the bacteria’s cell walls, popping them with simple brute force.”
Octapeptins are also effective in dissolving the mucus that bacterial infections like to thrive in, and that, he says, makes them a good candidate for combating lung infections.

Health & Medicine
Vaccinating newborns against the deadly rotavirus
“We are initially thinking that we might be able to use them in an inhaled powder for lung infections in cyctic fibrosis patients because in that form they stay in the lungs and don’t seem to be able to get into the blood stream and become too toxic.”
And that is the problem with octapeptins – they are such good killers that they are also good at killing us.
Once in the blood stream they quickly accumulate in the kidneys and overwhelm them. The good news is that Associate Professor Velkov and his collaborating researchers are finding that chemically altered synthetic octapeptin can potentially be kept out of the kidneys in mouse models.
In his previous work at Monash University, Associate Professor Velkov worked on a close relative of octapeptin antibiotics called polymyxins, that are similarly efficient bacteria killers but also toxic for the kidneys. Unlike octapeptins, polymyxins are used clinically but because they are so toxic they are a last resort drug. However, backed by five years of funding from the US National Institutes of Health, Associate Professor Velkov and colleagues were eventually able to create a synthetic version that is potentially safe in humans but hasn’t yet been clinically tested.

But because polymyxins are already in use, even if rarely, antibiotic resistance is already starting to emerge. “The clock is ticking on polymyxins, so we are going to need something else, which is where octapeptins come in,” Associate Professor Velkov says.
Octapeptins can not only kill bacteria susceptible to polymyxins, they can also kill the bacteria that are resistant to polymyxins. That is because octapeptins are a particularly virulent by-product of fratricidal bacterial warfare. Soil bacteria originally evolved polymyxins to ward off competitors, but to then stay ahead of each other, some went on to develop octapeptins to kill their relatives.
“Octapeptins are a great way to kill your close relative if they invade your feeding patch,” says Associate Professor Velkov.
But even if octapeptins pack a bigger punch that polymyxins, Associate Professor Velkov warns that nothing will stop bacteria building resistance to it because they are such simple and tough organisms.
“Bacteria are nature’s little beasts. They are incredibly robust single cell organisms that can super-efficiently do all they need to do – eat and multiply,” he says.
“But it isn’t all gloom and doom. We can stay ahead of resistance. Our nature’s well of compounds hasn’t dried up and there is a lot out there to be discovered and worked on. The biggest problem is there just isn’t any money in antibiotics.”

Sciences & Technology
The tiny drop fighting the big problem of antibiotic resistance
Antibiotics aren’t an attractive commercial proposition because they are a “one shot” medicine that resistance can soon make redundant. And that, along with overuse, is why resistance has reached crisis proportions. “We are running out of medicine because we’ve left the cupboard bare.”
In response to the crisis, governments and other agencies are increasingly offering upfront grants to partner with pharmaceutical companies in the development of new antibiotics.
“My biggest frustration isn’t the science or the knowledge because I know we can get there. My biggest frustration is being unable to translate what we know into real medicines on the shelf.
“All this knowledge is useless unless we can get industry involved to make it happen.”
Banner Image: Scanning electron micrograph of Penicillium mould producing spores. Picture: David Gregory & Debbie Marshall/Wellcome Collection