
Health & Medicine
Why mindset matters for junior doctors

A new report investigates the future of Australia’s medical workforce and finds a number of pressures, like increasing costs and digital disruption, are changing the way doctors deliver care to patients
Published 19 May 2019
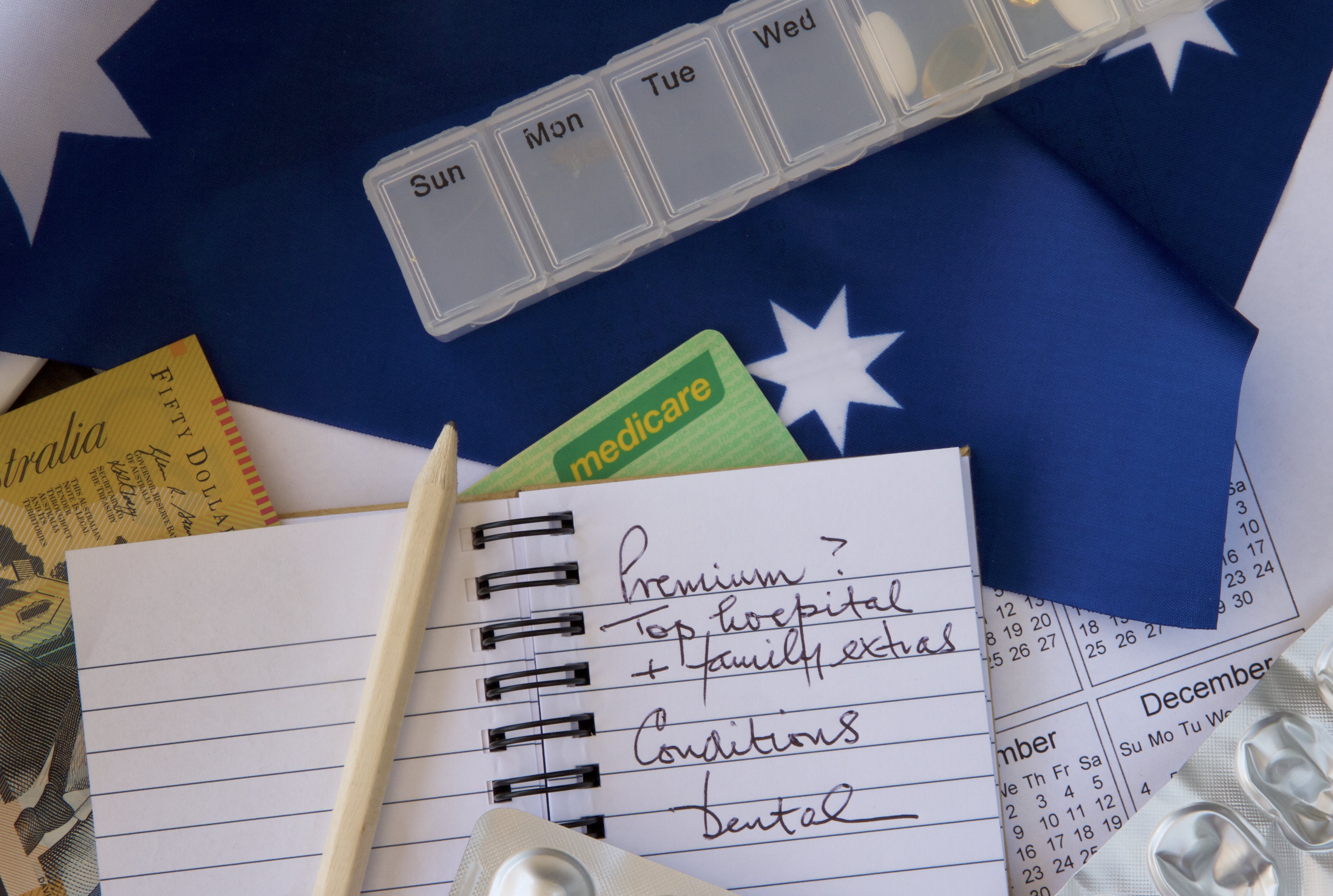
As Australia’s health expenditure continues to grow,currently at A$181 billion and 10.3 per cent of our Gross Domestic Product, governments and health insurers are increasingly concerned about both the growth in spending and its value – whether this growth is delivering improved health outcomes and access for the population.
This also reflects the concerns of the average Australian, including high out-of-pocket costs, the value of private healthcare, and persistently longer public hospital waiting times.

This mix of issues reflects the complex structure of our healthcare system, the changing patterns of disease (especially the increasing prevalence of chronic disease), high public expectations and technological change.
Within this context, our new ANZ-Melbourne Institute Health Sector report focuses on the future of the country’s medical workforce.
Doctors are a major part of the health system and play a key role in delivering high-value healthcare. The diagnoses they make and the treatments they recommend directly influence costs, quality and health outcomes, as well as driving other areas of spending like pharmaceuticals and hospitals.

Health & Medicine
Why mindset matters for junior doctors
But doctors are also facing a number of trends and challenges that are influencing the way they work, where they work and the care they provide.
The first challenge is the increase in the number of doctors – the number of medical graduates has more than doubled from around 1,400 in 2000 to 3,500 now.
As a result, the number of junior doctors has increased by an average of 8.9 per cent per year since 2005, and the overall growth in the total number of doctors is sitting at 5.3 per cent per year.
This is creating a much more competitive career ladder for doctors.
Medicine has always been competitive, but this increase in competition for coveted specialty training places will flow through to competition for jobs once they’re qualified. Junior doctors are increasingly reporting stress and burnout, mental health problems, bullying and gender discrimination, while female doctors have a higher rate of suicide compared to the general population.

There’s already some evidence that changing the culture of medicine could improve patient’s health outcomes, which in turn puts pressure on governments, medical colleges and employers to work toward this goal.
The second challenge is that although there are more doctors, their earnings continue to rise.

Health & Medicine
Protecting patients and their doctors
In line with national wage growth, all types of doctors across most age groups, for both males and females and across most specialties, are sharing the average 1.8 per cent annual growth in median earnings per hour.
The increased number of doctors has obvious implications for healthcare costs, and it’s important that population health outcomes also increase in line with this increase in supply.
Doctors need to be working in specialties and locations where there’s an under-supply and a high need for healthcare, like in rural areas, or focusing on chronic disease.
How to best use these extra doctors is a key issue for current policy and the future health of the population.

The third challenge is the persistent gap in earnings between men and women.
This gap, with men’s earnings per hour between 43 per cent and 55 per cent higher than women’s, hasn’t changed over the past ten years, although there is some weak evidence that this might be narrowing.
Men’s working hours have fallen much faster than for women. In fact, for some women in some age groups their working hours worked have started to increase.

Business & Economics
Putting doctors under a data microscope
Hourly earnings for women GPs are growing faster than those of men. This could reflect increasing opportunities for women and/or their preferences to work more hours. Or it could reflect a slowly improving culture as the proportion of women in the medical workforce increases over time.
This increase in supply will impact on doctors once they complete their training and enter into independent clinical practice. Given tighter budgets in public hospitals, it could be that these extra doctors are more likely to spend time working in private practice.
But demand here could also be limited, especially given the current issues concerning out-of-pocket costs and the value of private health insurance that is leading to a fall in private sector hospital admissions.
More competition in the private sector could lead to more consolidation of private medical practices – practices being merged with or sold to larger corporates in order to reduce costs – which could lead to higher fees and reduced access to care for patients.
Technology isn’t only influencing diagnosis and treatment but is also producing much more information and data that needs to be channelled into improved health outcomes and the lowering of costs.
With doctors taking up digital technologies, barriers such as privacy, medico-legal concerns and the effects on workflow need to be addressed.

Health & Medicine
Taking the pulse of general practice
There’s also the challenge of how doctors will use this technology and information compared with other health professionals, as diagnoses become more automated through artificial intelligence, and the time it takes to provide care falls – all of which have implications for fees, skill mix and increases in productivity.
Shared medical records like My Health Record have considerable potential to reduce waste and repetition, and could help increase much-needed co-ordination of care for patients with complex conditions.
Technology will also bring doctors and patients together online more often; benefiting those living in rural areas where access to medical is limited. But again, uptake, regulation and funding are key issues in ensuring that these technologies benefit patients at lower cost.
The current increase in the number of doctors will have far reaching impacts on medical care and the health system.

It seems clear that increased supply will alter the trajectory of medical careers, though strong policy is needed to ensure doctors work in specialties and localities with the highest need to maximise improvements in population health.
Improving the culture of medical training is necessary and will have positive impacts on the quality of care and the mental health of doctors, and potentially reduce the gender earnings gap.

Health & Medicine
The economics of good health
As doctor’s earnings continue to increase, more competition in private medical practice could place pressure on costs, and so it will be necessary to monitor these trends and their impact on patient’s access to care.
The use of digital technologies and shared records hold much promise, but need to be used for those most in need of healthcare, and carefully evaluated for their impact on population health and access to care.
Together, these challenges and trends will change the nature of doctor’s work and the markets in which they operate.
Given doctor’s central role in the healthcare system, ensuring these changes will benefit patients whilst keeping costs under control is a key issue.
Banner: Getty Images