Health & Medicine
Following cancer’s status updates

Precision medicine allows us to develop treatments for a specific disease in one person. But we must ensure all Australians can access these benefits
Published 1 November 2023
On this planet of more than 7.8 billion people, there’s no one quite like you. Genetically speaking, that is.
That’s why the future of cancer care is personal – tailored to fit the distinct variations in your genetic blueprint.
Until now, cancer treatments have been largely reliant on surgery, or chemotherapy and radiation, designed to shrink and kill cancerous cells.

In the age of ‘precision medicine’, we’re moving towards a more targeted approach, adopting drugs and therapies designed to seek out and shut down the changed or mutated proteins that cause cancer cells to grow, divide, and spread.
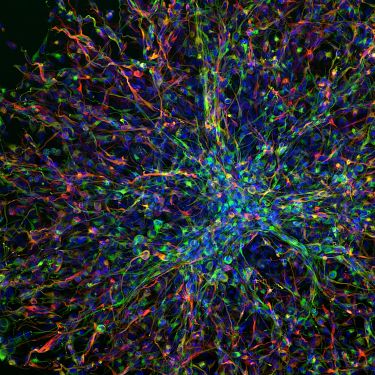
To understand what is causing a tumour and target its Achilles heel, we need to create a detailed map of a patient’s DNA – much like completing a complex jigsaw puzzle with more than six billion pieces.
We simply haven’t had the technology to put the pieces of the puzzle together until recently.
Health & Medicine
Following cancer’s status updates
When I sequenced the genome of an Australian cancer patient for the first time back in 2010, it took 50 people more than seven months, at a cost of more than one million Australian dollars.
We needed 16 machines to generate the data in 12 batches that took two and a half weeks each to complete.
Fast-forward to now and the rapid advances in machine learning, nanotechnology and big data mean a single machine like the Illumina NovaSeq 6000 can decode the genome of 48 cancer patients in less than two days, each at the price of an MRI scan.
Just like silicon chips transformed the way we use computers, new-generation sequencing technology is about to completely revolutionise how we research and design cancer treatments.
The ability to read genetic code can help with everything from tracking infectious disease outbreaks to prevent the next pandemic, to developing sustainable food crops to reduce world hunger.
Some of the greatest advances will be in health care, where this technology is already benefiting patients.
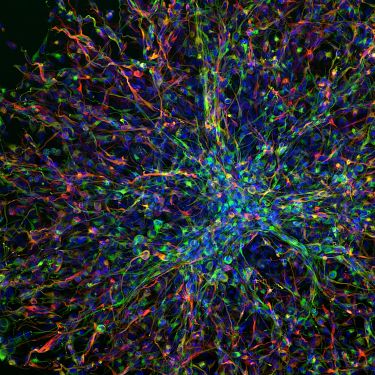
My research at the University of Melbourne Centre for Cancer Research focuses on sequencing genomes in real-time for patients with some of the rarest and most challenging types of cancer.
Health & Medicine
The Global Cancer Atlas
The results of these genetic tests are analysed through a series of round-table discussions between genetic data curators, scientists, expert pathologists and clinicians, who use the information to form specialised treatment plans and build a robust evidence base to help patients access clinical trials.
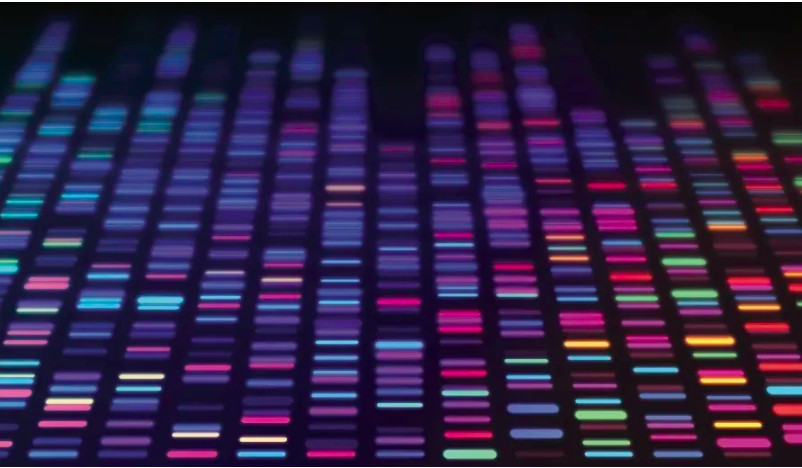
We are also pioneering a new way to collect tumour information from a simple blood test called a ‘liquid biopsy’. This method deciphers small amounts of cancer-specific genetic mutations in the bloodstream known as circulating tumour DNA (or ctDNA).
While a tissue biopsy requires specialised equipment and trained radiologists, a blood sample can be taken at most clinics by a nurse or phlebotomist, meaning people living in remote communities don’t have to travel long distances to access advanced imaging and surgical biopsies to diagnose, treat and monitor their cancer.
Once we map a patient’s genetic code, the information can help us figure out what type of cancer they have, where it originated in the body and what might have caused it to grow.
Then the matchmaking process begins.

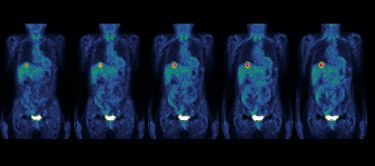
We take everything we have learned about a person’s cancer profile and compare it to available drugs, looking for treatments that exploit genetic vulnerabilities in their tumour cells.
The information embedded in a person’s DNA can also tell us if there is something in their metabolism that could cause them to have an adverse reaction to a medication, or whether a drug that works on one person will have little to no effect on someone else.

Health & Medicine
Our genetic strength in numbers
It can help us find the safest and most effective drugs for each patient, saving valuable time in their treatment and sparing them the side effects of trialling things that might not work.
Using genomic profiling to match patients with accurate treatments could also save the Australian healthcare system billions of dollars on ineffective prescriptions every year – creating a more sustainable and affordable system.
One of the questions I get asked more than anything else is ‘how close are you to finding a cure for cancer?’
When people hear about the incredible advances being made in science and technology, they wonder why we still haven’t been able to find a solution to a disease more than 150,000 Australians are diagnosed with every year.
The truth is, there’s no such thing as a singular ‘cancer’ to cure. Every person is different, and so is their disease.

Genomics-informed precision medicine is about understanding cancer at an individual level and doing our best to conquer the disease in that one person.
We don’t always have a drug that effectively targets the specific mutations in every person’s cancer type, so we need to treat them as best as we can with existing non-directed therapies and continue innovating to push new treatments down the pipeline.
We share what we’ve learned with other researchers around the world, collating summaries and blueprints of prior patients and developing detailed knowledge bases to work from for future cases.
Health & Medicine
Will Australia be left behind in the cancer genomics revolution?
My research team has provided genomic sequencing to more than 1,250 patients with rare and aggressive tumours through the Advanced Genomics Collaboration Clinical Genomics Platform.
It’s a start, but when you consider more than 100 Victorians are diagnosed with cancer every day – it’s clear we need to do more.
To unlock the true potential of genomic-driven cancer care and make precision medicine more affordable and available, we need to grow at scale.
That’s why the University of Melbourne has partnered with global biomedical company Illumina, to combine their next-generation sequencing technology with the research expertise and infrastructure needed to move genomics beyond the lab, into routine clinical care.

We have also signed an memorandum of understanding (MOU) with the Peter MacCallum Cancer Centre working towards establishing a new centre to transform how genomics and precision oncology is delivered in Australia.
The model will be unique in the Asia Pacific region, bringing together both organisations’ world-leading cancer, genomics and precision medicine experts into a unified group.

Health & Medicine
Unmasking cancers with hidden identity
For precision medicine to live up to its potential, we need to build strong foundations.
That means ensuring the data we collect is equitable and representative, for example, the current model is deeply skewed towards Caucasian samples.
While teams like the National Centre for Indigenous Genomics – led by Professor Alex Brown at the Australian National University (ANU) – are trying to correct this, not enough has been done to ensure Indigenous Australians are adequately represented in the data used as the building blocks of the precision medicine movement.
With Aboriginal Victorians twice as likely to be diagnosed with cancer than other Victorians and three times as likely to die from the disease, all researchers and institutions need to do more to ensure they don’t miss out on access to genomic medicine.
We also need to get the funding model right.

While some molecular tests looking at a small subset of genes are currently covered by Medicare (Australia’s universal health insurance scheme) – comprehensive whole genome sequencing tests are not, leaving Australia at risk of lagging behind the standard of care in many other countries around the world.
If we get it right, precision medicine is an incredible opportunity.
It can lead to better patient outcomes and a more efficient and effective healthcare system. While huge advances in technology mean our capacity to provide genomic-informed personalised cancer care is rapidly expanding, we have work to do to ensure all Australians can reap the benefits.
This research is part of The Advanced Genomics Collaboration (TAGC), a partnership between Illumina and the University of Melbourne to increase genomics innovation, its translation and adoption into the healthcare system and improve patient outcomes.
Banner: Getty Images