
Health & Medicine
What malaria can tell us about ‘switching off’ diseases like HIV
Scientists have discovered a new human autoinflammatory disease that causes repeated episodes of debilitating fever and inflammation
Published 12 December 2019
Every minute of every day our bodies are bombarded with millions of different molecules that we breathe, eat and touch including bacteria, viruses, chemicals and seemingly harmless compounds like food and pollen.
For every one of these encounters, our immune system has to decide if the substance is a threat or not, if it is ‘foreign or self’ and how the body should respond to stay healthy. To do this, we rely on two immune systems working in tandem.

Scientists have discovered a new human autoinflammatory disease that results from a mutation in an important gene in one of these systems.
The syndrome, now known as CRIA (cleavage-resistant RIPK1-induced autoinflammatory) syndrome causes recurring episodes of debilitating and distressing fever and inflammation.

Health & Medicine
What malaria can tell us about ‘switching off’ diseases like HIV
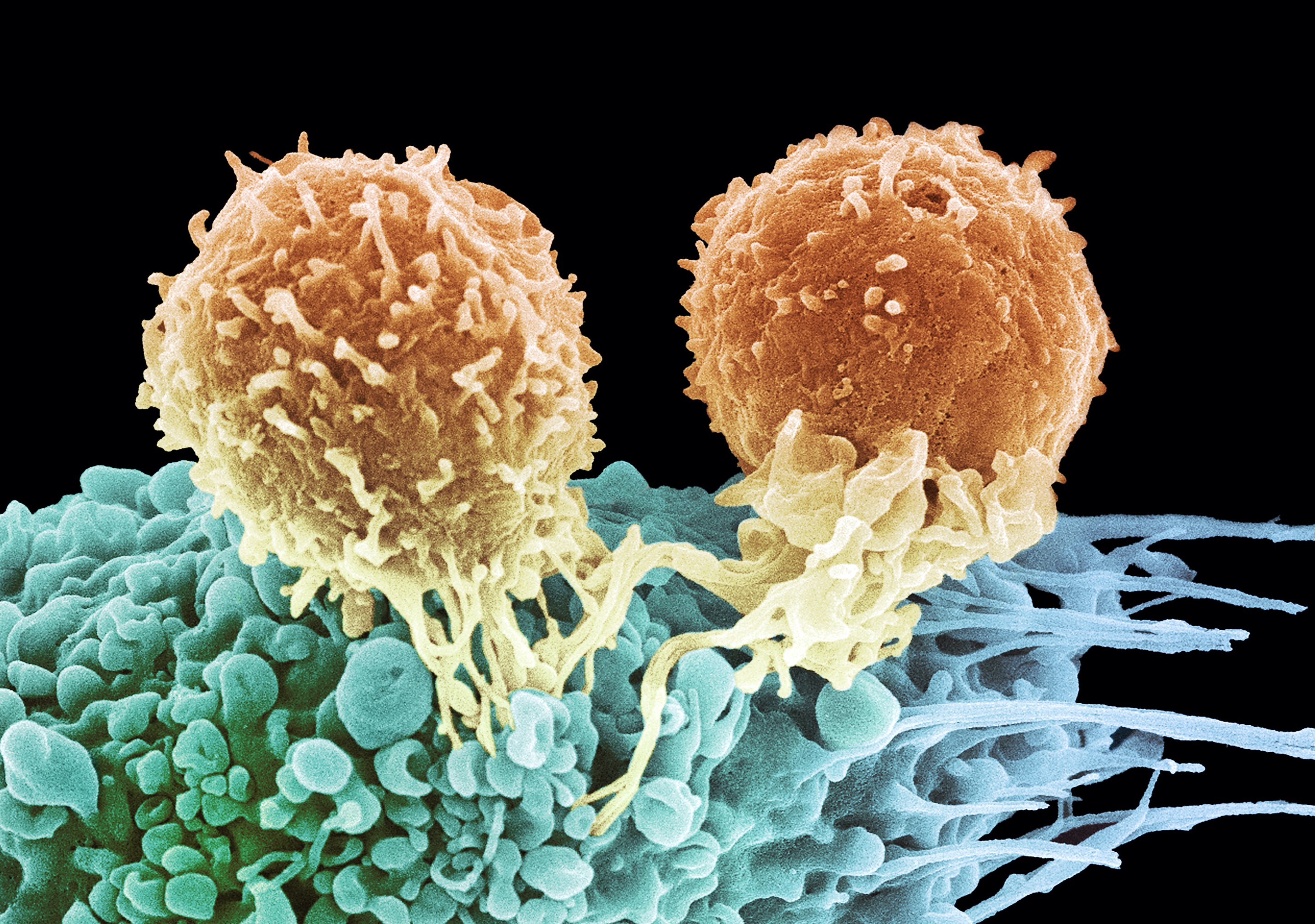
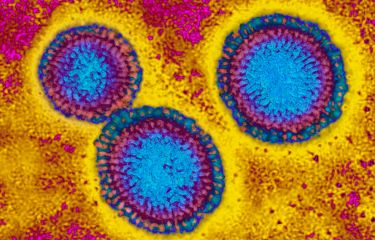
Our body’s first line of defence is the innate immune system that is effectively a ‘hard wired’ and fast response, explains Dr Najoua Lalaoui from the Walter and Eliza Hall Institute of Medical Research (WEHI) and the Department of Medical Biology at the University of Melbourne.
“This system works in the skin and mucous membranes like the mouth, making sure that any invaders like bacteria are detected and destroyed quickly,” she says.
If pathogens do enter the body, the innate immune cells move to the site of infection and physically devour invaders and activate chemical messengers to alert the body.
This can lead to an inflammatory reaction where blood circulation is increased, the affected area becomes swollen and hot, and the person may experience fever. When these chemical messengers are over-active it can result in conditions like colitis, arthritis and psoriasis.
Supporting this system is the ‘adaptive immunity’ system that involves antibodies that recognise and then train the body to respond to threats. This is our ‘memory immunity’ and the basis of how vaccinations work.
Scientists from the WEHI, with colleagues at the National Institutes of Health (NIH) in the United States, have been working to understand why patients from three families suffered from a history of painful swollen lymph nodes, fever and inflammation.
The families had a range of other inflammatory symptoms which began in childhood and continued into their adult years.
Health & Medicine
Defining a pathogen
“This type of repeated fever often indicates an issue with the innate immune system and the same disease in an extended family can indicate genetic changes that are passed from parents to their children,” explains Dr Lalaoui.
Previous tests didn’t identify any known cause.
But by sequencing the patients’ genomes, the NIH team identified a mutation in DNA that codes for a molecule known as RIPK that they suspected might cause the disease.
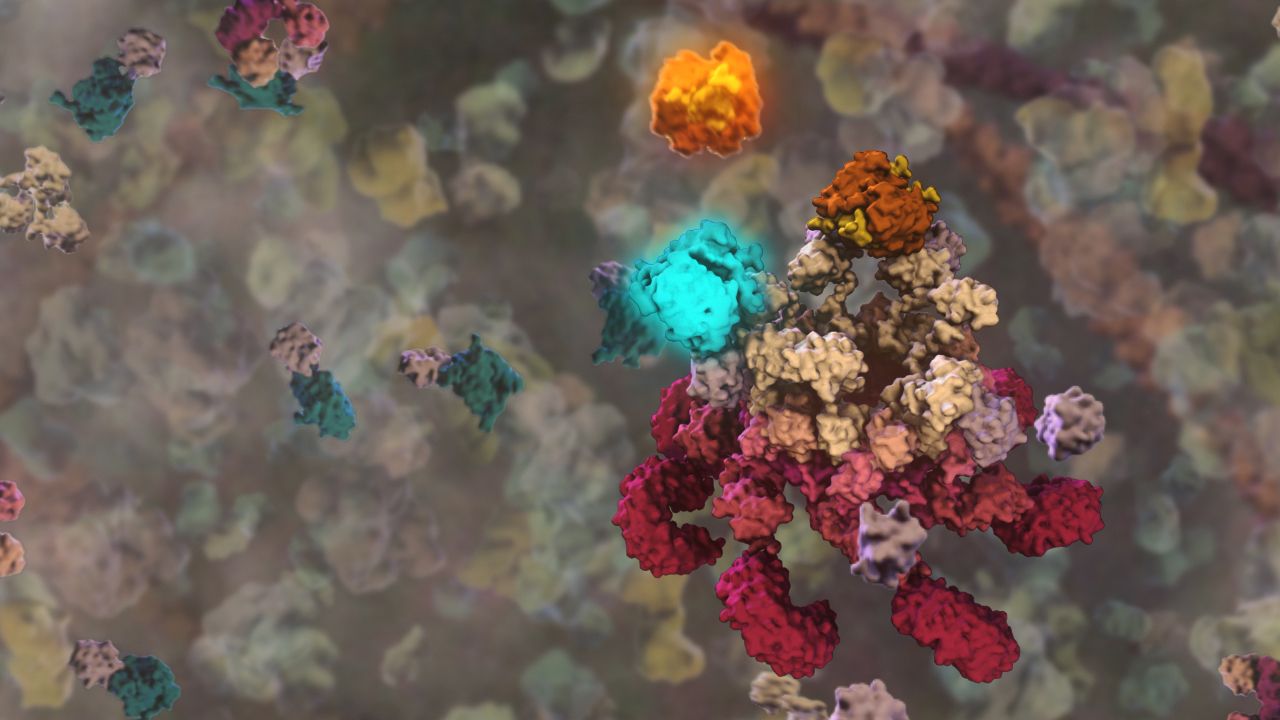
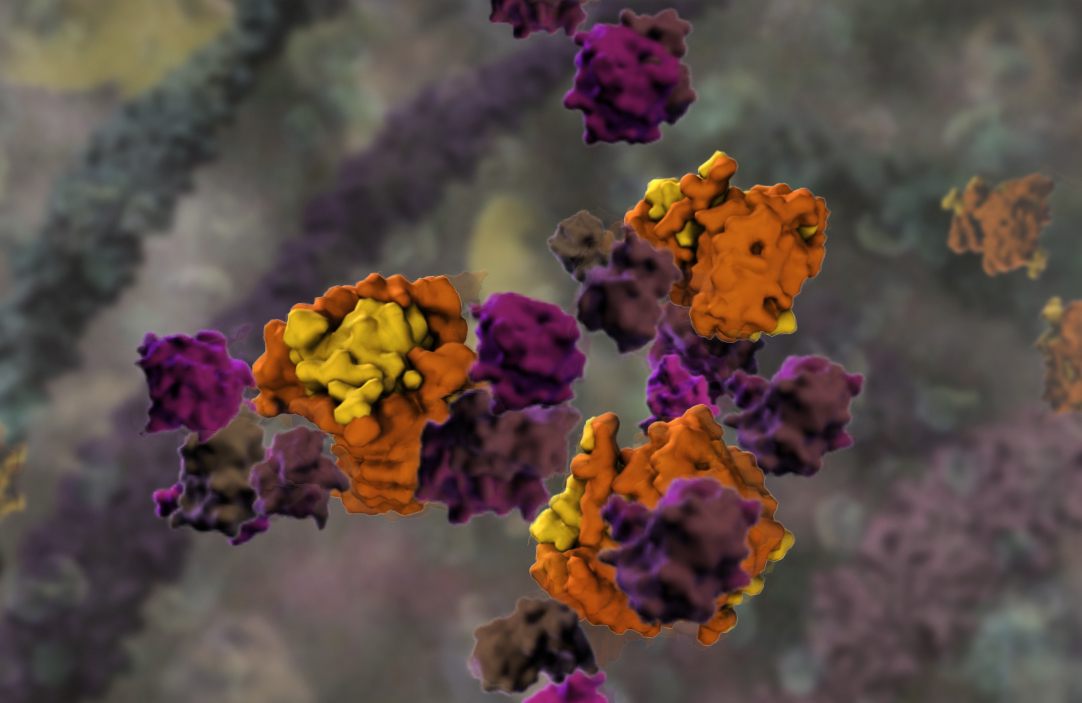
RIPK is a critical regulator of inflammation and the cell death pathway responsible for cleaning up damaged cells or those infected by pathogens.
Professor John Silke from the Walter and Eliza Hall Institute and his team have been studying RIPK1 for more than 10 years. His team had previously shown that damaging the RIPK1 gene could lead to uncontrolled inflammation and cell death.
“RIPK1 is a potent controller of cell death, which means cells have had to develop many ways of regulating its activity,” Professor Silke says.
“In this paper, we showed that one way that the cell regulates its activity is by cleaving RIPK1 into two pieces to ‘disarm’ the molecule and halt its role in driving inflammation.
“In this condition (CRIA), the mutations are preventing the molecule from being cleaved into two pieces, resulting in autoinflammatory disease. This helped confirm that the mutations identified by the NIH researchers were indeed causing the disease,” he says.
Health & Medicine
Our ‘killer’ cells’ role in life-long flu vaccine
He explains that mutations in RIPK1 can drive both too much inflammation –as in autoinflammatory and autoimmune diseases – and too little inflammation, resulting in immunodeficiency.
There is still a lot to learn about the varied roles of RIPK1 in cell death, and how we can effectively target RIPK1 to treat disease.
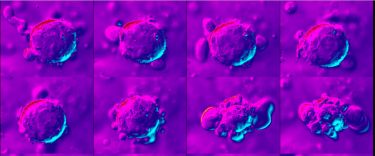
“In CRIA syndrome, the mutation in RIPK1 overcomes all of the normal checks and balances that exist, resulting in uncontrolled cell death and inflammation,” says Dr Steven Boyden from the National Human Genome Research Institute at the NIH.
Dr Boyden says the first clue that the disease was linked to cell death was when they delved into the patients’ exomes – the part of the genome that encodes all of the proteins in the body.
The team sequenced the entire exome of each patient and discovered unique mutations in the exact same amino acid of RIPK1 in each of the three families.
“It is remarkable, like lightning striking three times in the same place. Each of the three mutations has the same result – it blocks cleavage of RIPK1 – which shows how important RIPK1 cleavage is in maintaining the normal function of the cell,” says Dr Boyden.
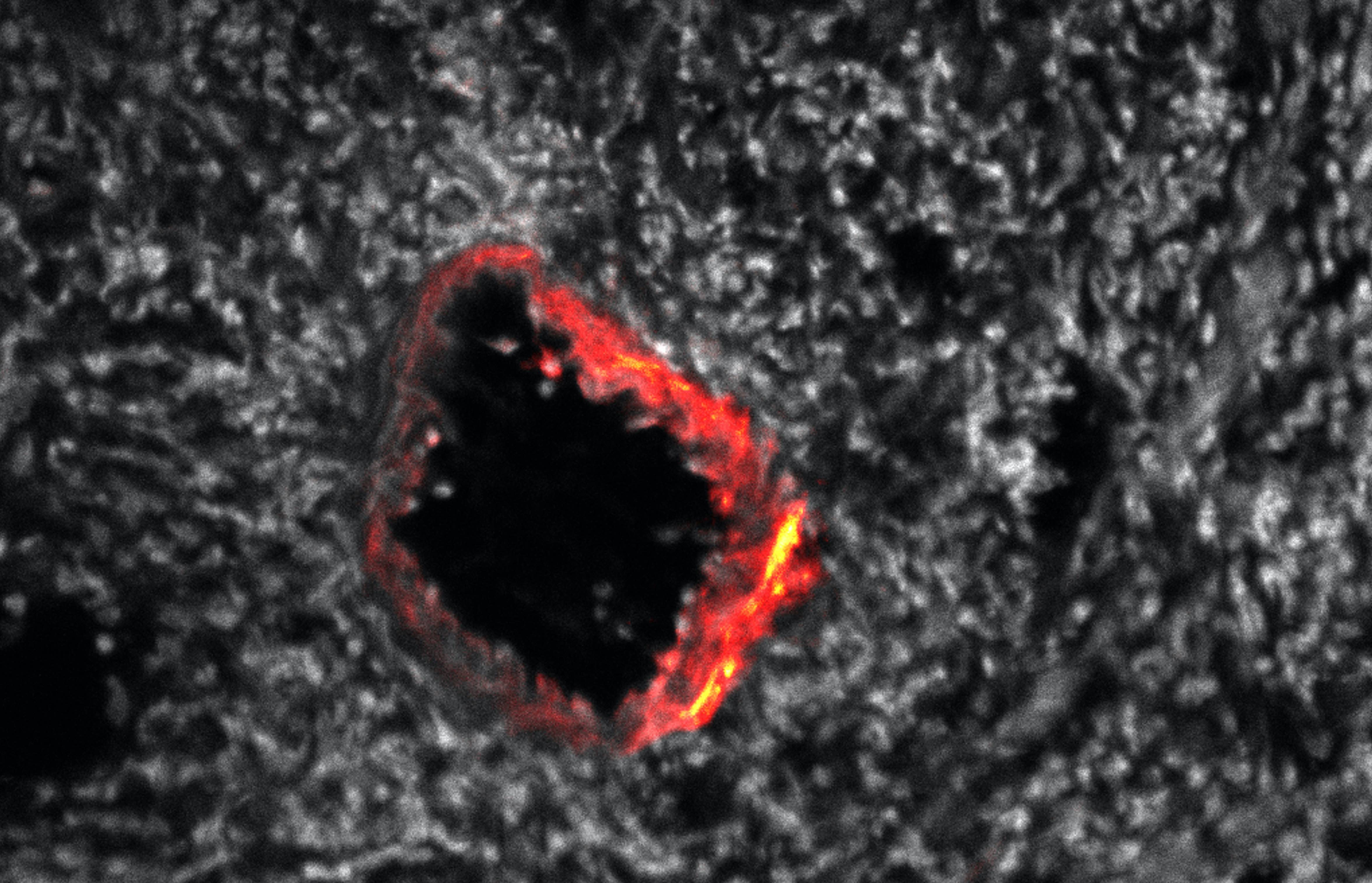
Dr Lalaoui said the WEHI researchers then confirmed the link between the RIPK1 mutations and CRIA syndrome in laboratory models.
Health & Medicine
Stopping healthy cells from self-destructing
“We showed that mice with mutations in the same location in RIPK1 as in the CRIA syndrome patients, had a similar exacerbation of inflammation,” she says.
Dr Dan Kastner from NIH – widely regarded as the father of autoinflammatory disease – says colleagues had treated CRIA syndrome patients with a number of anti-inflammatory medications, including high doses of corticosteroids and biologics, compounds that block specific parts of the immune system.
And although some of the patients markedly improved, others responded less well or had significant side effects.

“Understanding the molecular mechanism by which CRIA syndrome causes inflammation provides an opportunity to get right to the root of the problem,” Dr Kastner says.
Dr Kastner noted that RIPK1 inhibitors, which are already available on a research basis, may provide a focused, ‘precision medicine’ approach to treating patients.
“RIPK1 inhibitors may be just what the doctor ordered for these patients. The discovery of CRIA syndrome also suggests a possible role for RIPK1 in a broad spectrum of human illnesses, such as colitis, arthritis and psoriasis.”
Banner: WEHI