The immune legions fighting Legionnaires’ disease
Researchers solve immunity puzzle in lung tissue and reveal previously unknown ‘immune cell circuitry’ as secret weapon in front line defence against Legionella.
Published 16 June 2016
Researchers have uncovered a group of immune cells that work together to destroy Legionella bacteria in lung tissue, the front line in the fight against the deadly disease.
The discovery, which has been published in PLoS Pathogens, arose from a novel approach by University of Melbourne immunologists and microbiologists to investigate why some people are not affected by Legionella, while others have difficulty fighting it off.
Until now, it has been unclear how our immune system responds to this bacterium.
“Immunologists have tended to look at what is happening in the immune organs, such as the bone marrow, lymph nodes and spleen, because that is relatively easy,’’ says the study’s co-lead author Professor Ian van Driel, Head of Department of Biochemistry and Molecular Biology at University of Melbourne’s Bio21 Molecular Science and Biotechnology Institute.
“We have often ignored what happens in the actual infected tissue where the bacterium is destroyed.
“The right tools and markers to investigate how the immune system functions in tissues were not available until recently.
“In our study, we exploited new tools to understand how the ‘immunity puzzle’ fits together in lung tissue, and examined the complex cellular interactions that control the infection.”
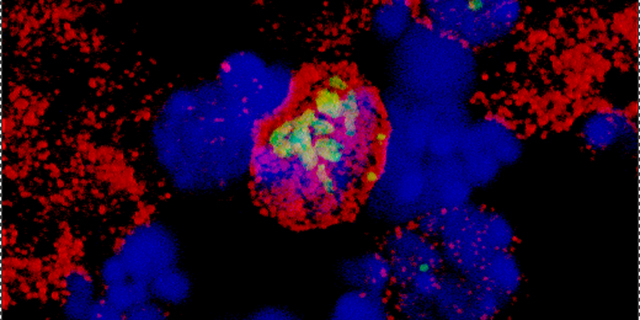
PhD student Andrew Brown, from the Department of Biochemistry and Molecular Biology at Bio21, utilised a recent Belgian study published in Immunity which characterised immune cell populations in inflamed tissues. He applied their methods to observe cellular activity in lung tissue infected with Legionella bacteria.

Brown uncovered a population of immune cells, known as monocyte-derived cells or MCs, which were found to play a significant role in fighting Legionella bacteria.
He was able to show that MCs responded to Legionella within 24 hours of infection. By 48 hours, the MCs outnumbered macrophages by 10 to 1.
Macrophages, a type of white blood cell important in fighting infections, were previously thought to be the major cell type that engulf and destroy bacteria.
“Rather than the macrophages, it was the MCs that were ‘gobbling up’ and controlling the bacteria. We didn’t even know that MCs were there, let alone in such large numbers. This was a surprising find,” he said.
The researchers found that once Legionella enters lung tissue, the innate immune system kicks in. MCs secrete a chemical messenger called interleukin-12 which fires off warning signals that rapidly stimulate other immune cells that are recruited to the lung. These cells produce large amounts of interferon gamma, another powerful chemical messenger of the immune system, which then instructs the MCs to kill the Legionella bacteria.
And all this happens within 48 hours.
Legionnaires’ disease is caused by an infection of the lung by the bacterium Legionella pneumophila. It is a form of pneumonia with symptoms including headaches, fever, shortness of breath, coughing and muscle pain.
It attacks very rapidly – within a day a whole population of Legionella bacteria can multiply in the lung. Understanding these complex cellular processes is critical to controlling the infection.
“Legionella causes disease in susceptible people by replicating inside their lung macrophages. This is not deliberate; the bacteria are ‘trained’ to replicate in environmental amoebe and they treat macrophages in the same way,” says co-lead author Professor Elizabeth Hartland, Head of the University of Melbourne’s Department of Microbiology and Immunology at the Peter Doherty Institute for Infection and Immunity – a joint venture between the University of Melbourne and Royal Melbourne Hospital.
“Legionnaires’ disease is a completely accidental infection.”
It doesn’t pass from person to person, but can be contracted by inhaling water droplets derived from contaminated water sources, such as air-conditioning cooling towers, spas and fountains.

Two people have died and more than 50 have been diagnosed with Legionnaires’ disease in New South Wales this year as health authorities wrestle with the deadly outbreak.
The elderly, smokers, and people suffering from cancer and chronic lung conditions, with compromised immune systems, are particularly vulnerable to the disease.
“Knowledge of this immune cell circuitry in the defence against Legionella shows us what an effective immune response looks like, and allows us to focus on how to manipulate and optimise the immune response to fight infection,” says Professor Hartland.
“With the rise of antibiotic resistance, this knowledge will give us new options to fight acute lung infections, such as Legionnaires’ disease, where we can strengthen the immune system and fight the infection at the same time.”
“It will also allow us to offer patients a more personalised and accurate prognosis for their infection, and give us vital information about when to use antibiotics.”
Banner image: iStock



