
Health & Medicine
Peer support groups connect people living with a brain injury

Traumatic brain injuries have devastating consequences for patients and their families, driving research for new treatments
Published 20 August 2024
Since their e-scooter trial began in 2022, Victorians have rapidly adopted this low-carbon, highly accessible, lower-cost mode of transport.
Although e-scooter hire was recently banned in Melbourne’s CBD, the trial continues in the inner suburbs in addition to an estimated 100,000 and growing, privately owned e-scooters in Victoria.
Unfortunately, this is linked to a steep rise in emergency department hospitalisations.
Head injuries are one of the most common e-scooter-related injuries.
A Royal Melbourne Hospital study recorded head injuries in 50 per cent of e-scooter-related accidents, second to upper limbs at 53 per cent.
The study also found that only one-third of e-scooter riders who presented to the emergency department wore a helmet.
E-scooter head injuries are often severe, including traumatic brain injury.
In recent decades, the management of head injuries has improved our ability to prevent damage from getting worse, but treatments to actively enhance healing and recovery have not changed significantly.
This increased rate of injuries is a timely reminder that new techniques are desperately needed.
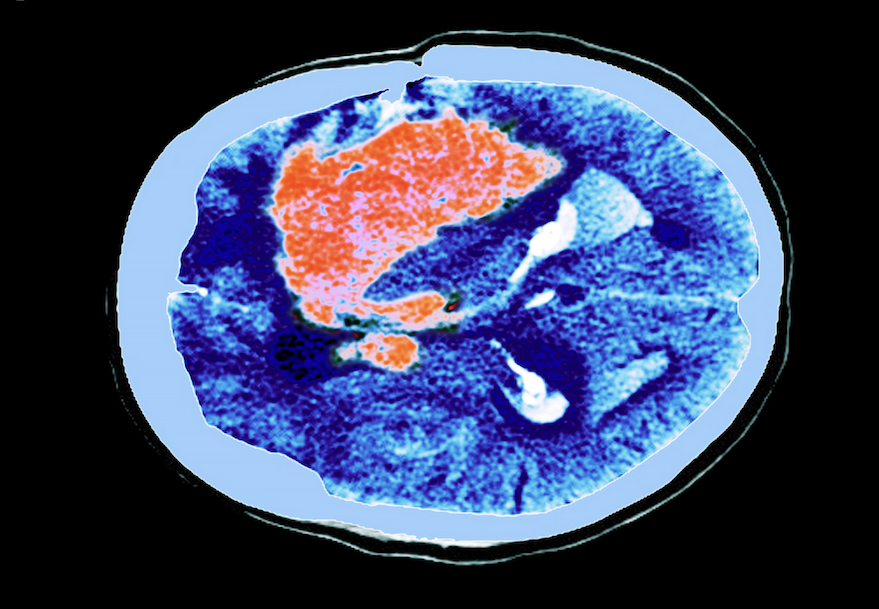
Characterised by a blow or other force to the head, a traumatic brain injury (TBI) results in damage to the brain or an alteration in brain function.
The leading causes of TBI in Australia are transport accidents, falls and collisions with objects.
TBI can cause long-term physical disability and complex neuro-behavioural effects that disrupt quality of life, including neurological impairment (motor function impairment and sensory loss).
Other changes can include medical complications (including spasticity and post-traumatic epilepsy) and cognitive impairment (memory impairment and problems with planning, language and safety awareness).
TBIs can lead to personality and behavioural changes (including impaired social and coping skills) and lifestyle consequences which can result in unemployment, difficulty maintaining interpersonal relationships and loss of independence.
Current medical intervention is limited to stabilising the patient and optimising their physiological parameters including intracranial pressure, oxygenation, blood pressure and blood glucose.
Despite these interventions, neural cells die from the physical damage, beginning a sequence of events that creates inflammation. As a result, the patient has little scope to improve neurological function and an extremely decreased quality of life.

Health & Medicine
Peer support groups connect people living with a brain injury
TBI is the major cause of death and disability in individuals under 25 in industrialised countries.
A 2008 report by Access Economics estimated 1,493 new cases of moderate TBI and 1,000 cases of severe TBI in Australia, per year. Of which, 22.6 per cent for moderate TBI and 35.1 per cent for severe TBI would die within 12 months post-injury.
In Australia, patients are typically young males who are disabled for the remainder of their lives. Of the 700,000 Australians currently living with a brain injury, 66 per cent acquired their injury before the age of 25, and 75 per cent are men.

Compared to bicycle injuries, patients who sustained injuries related to scooters are more likely to be under the age of 18 (26.7 per cent compared to 16.4 per cent).
Without effective treatment, TBIs represent an enormous challenge in terms of life-long care and management, with estimated lifetime costs between AU$2.5 million and AU$4.8 million per individual.
Considering the increasing popularity of e-scooters and the rise of associated injuries, it is a crucial time to consider the treatment landscape for TBI.
Despite advancements in post-TBI care in terms of better intensive care units and improvements in post-TBI rehabilitation, the last major improvement in the immediate care of severe traumatic brain injury patients occurred over 40 years ago.
This was when computed tomography or CT scanning was included as part of routine assessment and treatment.
However, this only provides a window into the brain, providing clinicians with a clear picture of TBI severity to help guide rehabilitation.

Although advancement in therapeutics to date has been elusive, it has not been without effort.
Many potential treatments have been developed but failed to improve clinical outcomes for severe traumatic brain injury patients.
To address the need for new TBI treatments we have formed a multidisciplinary team including neuroscientists, trauma clinicians, neurologists, medicinal chemists, pharmacologists, biochemists, medical engineers, health economists and advisors.
Our goal is a targeted therapy to sustain neural function, to maintain homeostasis (a stable condition) and to remodel and repair the brain.

Health & Medicine
Why your brain health matters
The solution builds on our pioneering work in injectable hydrogels for brain repair and scaffold design to reduce inflammation and promote neural regeneration.
These soft gels allow precise and minimally invasive placement into the brain lesion.
The injected liquid fills the irregularly shaped lesion from the injury and rapidly reforms a soft matrix with similar mechanical properties to the surrounding brain tissue.
The hydrogel forms a permanent, biocompatible matrix to stabilise the injury.
This is crucial as the adult brain cannot regenerate the cerebral extracellular matrix (a 3D network that surrounds brain cells, providing mechanical support and protection to the brain tissue), particularly within large lesions, characteristic of severe traumatic brain injury.

When implanted, the hydrogel reduces inflammation, and stabilises the damaged tissue creating a microenvironment for brain cell survival and neural network formation; in effect, repairing the damaged brain.
In as-yet-unpublished research with animal models, we found the implanted hydrogel decreased brain inflammation and improved motor function 28 days after traumatic brain injury.
The first-generation patented hydrogel device has pre-clinical validation, and we will complete Pharmacokinetic-Pharmacodynamic (PKPD) analysis, toxicology analysis and primate experiments to progress to a Phase I (safety) trial in the next five years.
This promising new clinical protocol offers a new era of treatments for TBI to drastically improve patient outcomes and reduce the economic burden on patients, their families and the Australian health system.
And this could not be more timely.