Health & Medicine
The science behind the search for a COVID-19 vaccine

Every one of us is at risk of being both a potential COVID-19 patient and virus vector, with about 20 per cent being ‘super spreaders’. Electing to be vaccinated fulfils a very basic responsibility to ourselves, our family and the community
Published 10 December 2020
This article is the latest in a series of weekly columns about all things infection and immunity written by Nobel Laureate Professor Peter Doherty for the Doherty Institute, Setting It Straight.
The disease we call COVID-19 is a confrontation between a very small, rapidly multiplying invader (SARS-CoV-2) and the (by comparison) enormous, long-lived, slowly-reproducing, multicellular, multi-organ system we call a human being.
Accessing our upper respiratory tract in the air we breathe, the outer spike protein of the SARS-CoV-2 virus attaches to the physiologically important (and ubiquitous) angiotensin converting enzyme-2 (ACE2) molecule expressed on our respiratory epithelium.

That binding event tricks the cell into internalising the virus particle (virion) where, once in, the viral RNA is released and, with the co-option of some of our genes, the process of replication and producing new virions gets under way.
Health & Medicine
The science behind the search for a COVID-19 vaccine
The extent to which newly made virions increase in numbers and penetrate deeper into the lung – or are distributed via the blood to other body organs – dictates the ‘pathogenesis’ and clinical severity of COVID-19.
Virus breathed-out or, more violently, sneezed and coughed into the air, determines the extent of person-to-person spread, the ‘epidemiology’ of the infection. Both aspects of virus dissemination are brought to an end when the adaptive immune response we’ve been discussing at length does its job.
The expectation with vaccines is, of course, that they will prevent, or at least ‘jump start’ the immune termination of the infectious process, to limit the extent of virus induced pathology (damage) within the individual and, externally, to break the virus transmission chain across the broader community.
In fact, we are talking about the virus induced compromise of two complex, interlinked human ecosystems; one internal to us that involves the expertise of the physician and pathologist, the other external that requires the skill sets of the epidemiologist, the public health professional and the formulation of clear and effective policy at the political level.

You may not think of yourself as an ‘ecosystem’, but it’s no coincidence that much of the mathematical modelling of how viruses and immunity interface within us (initiated during the HIV/AIDS pandemic) uses modelling approaches developed earlier by Oxford UK-based Australian physicist, then zoologist Bob (Lord Robert) May to analyse predator/prey relationships in rural environments!
Health & Medicine
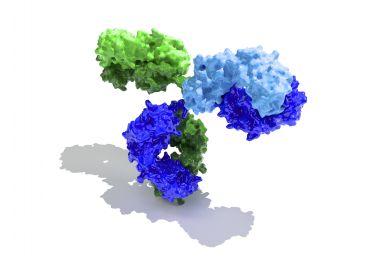
Your protective Igs: The major focus of COVID-19 vaccines
Every one of us is at risk of being both a potential patient (though some can be asymptomatic) and a virus vector, with about 20 per cent being ‘super spreaders’. In electing to be vaccinated, we fulfil a dual, and very basic responsibility to ourselves, our close associates and family, and to the community at large.
Should we choose not to be vaccinated we side, perhaps unconsciously, with the SARS-CoV-2 virus and its evolutionary need to survive across the planet as a human pathogen that infects more and more people.
If you think that ‘herd immunity’ following natural infection can solve the problem, there’s a way to go with COVID-19.
Some 14 million or so ‘cases’ of COVD-19 are currently acknowledged across the USA. Even if we think that another 14 million may have been missed, 90 per cent or so of the population is yet to be infected! And, of course, the ‘protected’ peoples of Australia and New Zealand are totally vulnerable.
Personally, I think a lot of the objection to vaccines reflects that many don’t fully understand what happens in a virus infection. As a professional who has worked on viral pathogenesis and immunity for more than 50 years, it’s my job to do my best to convey that information better. Next week’s essay will focus on pathogenesis, on the ecosystem within.

The first thing to understand re vaccination versus infection is that, like any medical intervention (or crossing the street to get to the other side) this is a risk/benefit equation. There is always a finite risk, even if it is at a level of one in a million, or one in a billion.

Health & Medicine
Lessons for a future pandemic
No physician can assure you absolutely that a particular therapeutic (drug), vaccine or surgical procedure is totally without risk.
On the other hand, medical professionals are committed to the linked ideas of ‘duty of care’ and ‘first do no harm’, so they will not recommend a particular treatment if they are unconvinced of the likely benefit. And your doctor must inform you re possible risk before you sign any ‘informed consent’.
Apart from healthcare professionals, when it comes to something completely new like the SARS-CoV-2 vaccines, that risk/benefit equation will dictate the actions of commercial developers (no company wants to attract massive class-action suits and have its reputation trashed) and regulatory authorities.
Across the planet, the regulators are public employees, with the planetary benchmark being set by the US FDA, the Food and Drug Administration. Why is that? If any manufacturer wants to sell globally, they must have FDA approval. The FDA refused, for example, to approve the use of the drug Thalidomide by pregnant women, with the consequence that the USA avoided the catastrophe of babies being born with foreshortened limbs.

Among other criteria mandated by the FDA, the steps in testing a new vaccine must first pass the scrutiny of institutional (for example university) Animal and Human Experimentation Ethics Committees, which have some lay members, typically retired business owners, lawyers, teachers or preachers.

Health & Medicine
Gaining clarity on the ethical issues of a possible COVID-19 vaccine
And independent data-review processes must be built into every evaluation step – from the preclinical trials in laboratory animals to the escalating phase 1, 2 and 3 clinical trials in humans.
In the present emergency with COVID-19, some of that has been truncated to allow, for example, the preclinical and phase 1 (just injecting the vaccine to see if it is safe) trials to be run concurrently, but all that data must be available for the experienced FDA professionals to evaluate before approval is given for even limited emergency, as distinct from general, use.
And Australia’s TGA (Therapeutic Goods Administration) regulators will draw on a number of sources (including the FDA) to make their own, detailed analysis.
Once a vaccine is given to a couple of million people, beyond the 20,000 or so exposed in a phase 3 clinical trial where vaccinated (and placebo-treated) individuals are confronted by the possibility of natural infection, it is quite possible that safety concerns will emerge.
Some vaccinees will inevitably develop other disease problems, or even die. The task then is to determine if there is any link back to the vaccine. At the same time, we should also be seeing evidence of massive benefit, with the numbers of newly infected individuals dropping dramatically.
Next week, I’ll go on with the discussion of mechanism, and we’ll look at the difference between vaccination and infection from the perspective of pathogenesis and disease process in the ecosystem within.
Banner: Getty Images