Health & Medicine
Grasping COVID-19’s long neurological tail

There are many unknowns about the long-term effects of COVID-19 on the brain – but new research investigates the potential impact of Post COVID-19 Neurological Syndrome (PCNS)
Published 21 October 2020
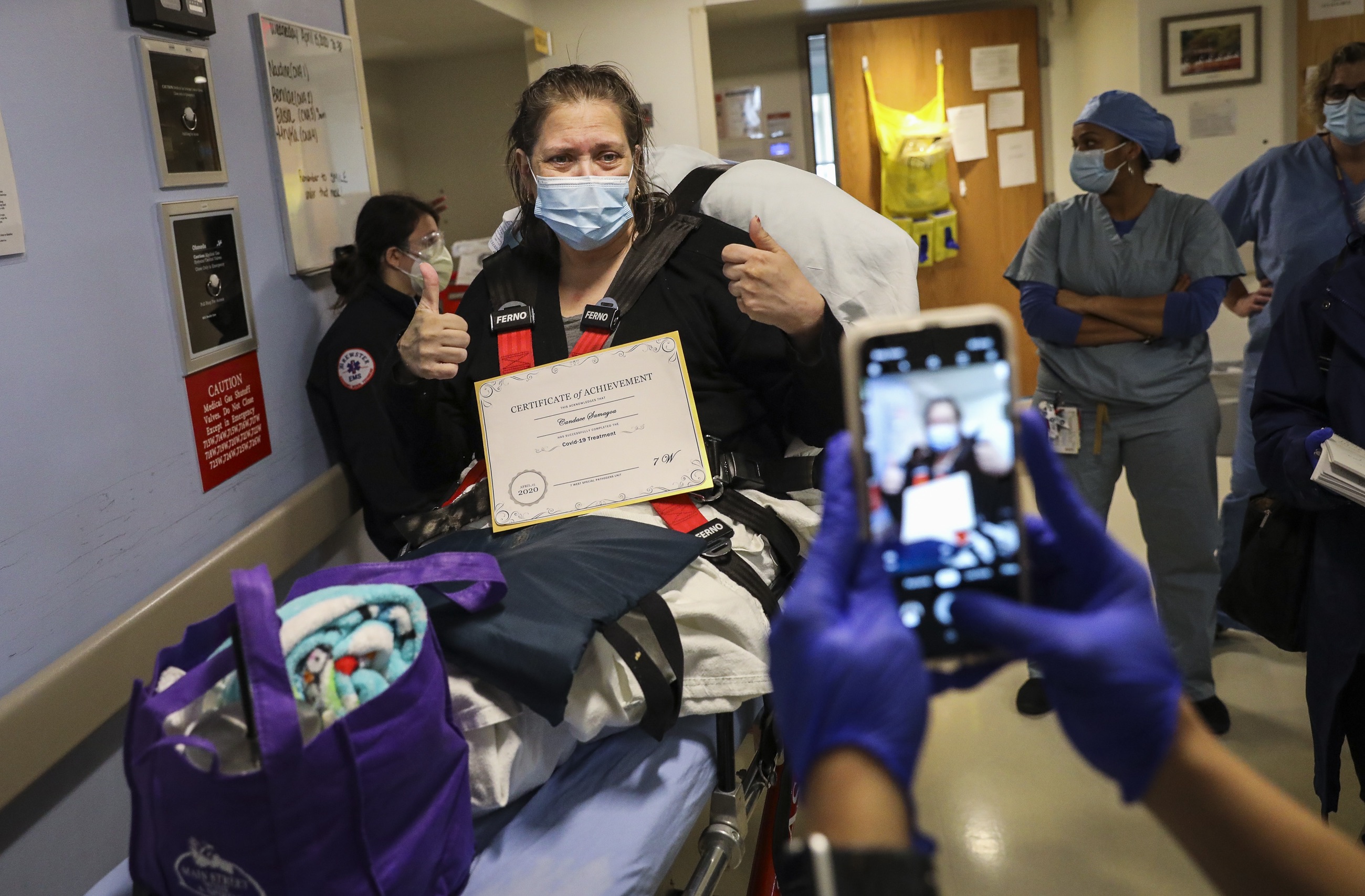
As the global COVID-19 pandemic continues, with currently more than 38 million COVID-19 cases worldwide, we’re beginning to understand the long-term impact of the virus on the human brain. Something we’re calling Post-COVID-19 Neurological Syndrome, or PCNS.
The symptoms are similar to those experienced post-stroke – but the age group is much younger – and, given the scale of global infection, PCNS has the potential to become a major problem.

The neurological impacts of various infections have been explored and investigated in the past, but as COVID-19 is a new virus, we are still working to understand the longer term impact of the infection.
Daily, more and more reports are appearing in the mainstream media of recovering patients describing lingering symptoms that won’t go away. In scientific journals, like Nature, research has found similar symptoms linked to earlier epidemics including the Middle Eastern respiratory syndrome coronavirus (MERS-CoV) and the severe acute respiratory syndrome virus (SARS-CoV).
Many people who have officially recovered from these viruses cite disabling chronic fatigue (that is, fatigue lasting more than six weeks) and a series of persistent attention and cognitive problems – similar to post-stroke symptoms such as fatigue, depression and apathy among patients.
Health & Medicine
Grasping COVID-19’s long neurological tail
If we look to Europe, a series of large online questionnaires focusing on COVID-19 recovery found that less than one percent of surveyed patients were symptom-free 79 days after the infection – which suggests the high likelihood of PCNS in over 90 per cent infected people.
The European survey involved more than 2,000 non-hospitalised younger COVID-19 patients and just over 100 hospitalised (but only mildly affected) COVID-19 patients with a mean age 47 years and good health before the COVID-19 infection.
To make matters more complicated, there are a number of re-infection reports emerging from different parts of the world, reminding us that there are still so many unknowns when it comes to COVID-19, post-COVID-19 issues and a potential vaccine.

The physical stress of infection might end, but COVID-19 patients can carry emotional and neurological scars from the experience for months and years, often in the form of post-traumatic stress disorder (PTSD).
For example a large Chinese study earlier this year revealed that an alarming 96.2 per cent of recovering COVID-19 patients have clinical evidence of severe post-traumatic stress disorder (PTSD).

Health & Medicine
Will COVID-19 change healthcare for stroke patients?
A total of 730 COVID-19 clinically stable patients were assessed and a large percentage – 96.2 per cent – were found be suffering from severe PTSD; something we believe is one of the first signs of PCNS.
Similar reports have previously been reported following the SARS epidemic in 2009. Almost 50 per cent of people recovering from the virus developed PTSD symptoms that were still evident four years after infection.
PCNS is real and what is beginning to emerge is the undeniable evidence of persistent long-term neurological and affective symptoms post-COVID-19.
Interactions between our immune system and the central nervous system are one of the most complex and interactive regulatory networks in mammals. So, the fact that the brain is affected by COVID-19 is not surprising.
Our research looked at the local and global immunological response to the viral infection with the help of readily available peripheral markers of inflammation such as neutrophil-lymphocyte ratio, CRP -and D-dimer.
We carried out an in-depth analysis of the neurological symptoms of several patients with COVID-19.
COVID-19 and acute stroke share common pathobiology at a cellular level.

Health & Medicine
COVID-19 distancing especially hard on those with mood disorders
The biological consequences of the virus in the lungs leads to the release of cytokines that increase in number as respiratory symptoms increase, often leading to a ‘cytokine storm’ affecting the vascular system and whole body, including the brain.
Hypercoagulation in the blood is associated with clots that can affect the brain in a similar way as an acute ischemic stroke. But early detection is important as these patients can be helped, and there are simple tests that appear to be quite useful.
Our brains decide and control how we feel, how we perform and how we get on with our day-to-day lives. So, disorders of the brain can have a significant impact on our lives and worldwide are the leading cause of disability.

And it’s worth exploring the likely mechanisms of SARS-CoV-2 (the virus responsible for the COVID-19) causing PCNS.
Our team have studied 14 patients with COVID-19 and brain involvement to date, and further studies continue.
Brain expression of SARS-C0V-2 entry point keyholes (receptors) and related proteins are well accepted, and a variety of studies have explored brain invasion by the virus and potential routes of entry.

Health & Medicine
Training your brain in lockdown
SARS CoV-2 has been shown to cause infection and inflammation of inner lining of the blood vessels within hours of acute infection.
This leads to an army of immune cells and chemicals released by these cells known as cytokines to be unleashed inside the local blood vessels . These chemicals can reach the brain within minutes, affecting the endothelial cells of the blood brain barrier (BBB) which makes it easier for the virus and large molecule chemicals to enter.
To date, our team has found significant similarity between the pathobiology of stroke and COVID-19 involvement in the brain. Our previous research found cytokine-mediated post-stroke depression and post-stroke fatigue to be the norm rather than the exception.

And we believe the same is true of PCNS. So, there must be a plan and clinical trials now as a matter of urgency.
PCNS appears to show clinical features like persistent fatigue, depression, chest pain and tightness, muscle pain, anxiety, sleep disorders, an inability to concentrate properly (which some patients describe as ‘brain fog’), apathy and more.
Will these be persistent for several years to come? Possibly. Can these symptoms be cured? We like to think so.

Health & Medicine
The brain benefits of music
But awareness is key.
GPs and neurologists must be vigilant for PCNS. Simple blood tests such as neutrophil-lymphocyte ratio and C-reactive protein allow easy monitoring of persistent inflammation.
Our team is now in the process of finalising our study protocols to run clinical trials to treat PCNS patients early.
Understanding and treating the neurological effects of COVID-19, as well as the potential scale of the problem, is critically important as the pandemic continues in the coming months or even years.
If you’ve had COVID-19, please consider participating in clinical trials that may help you and others. For more information contact the team: twi@unimelb.edu.au
Banner: Getty Images