
Health & Medicine
Rethinking gastrointestinal cancer diagnosis
Using four different approaches, researchers are attacking one of our most prevalent and preventable cancers, with the common goal of saving thousands of lives
Published 15 June 2020
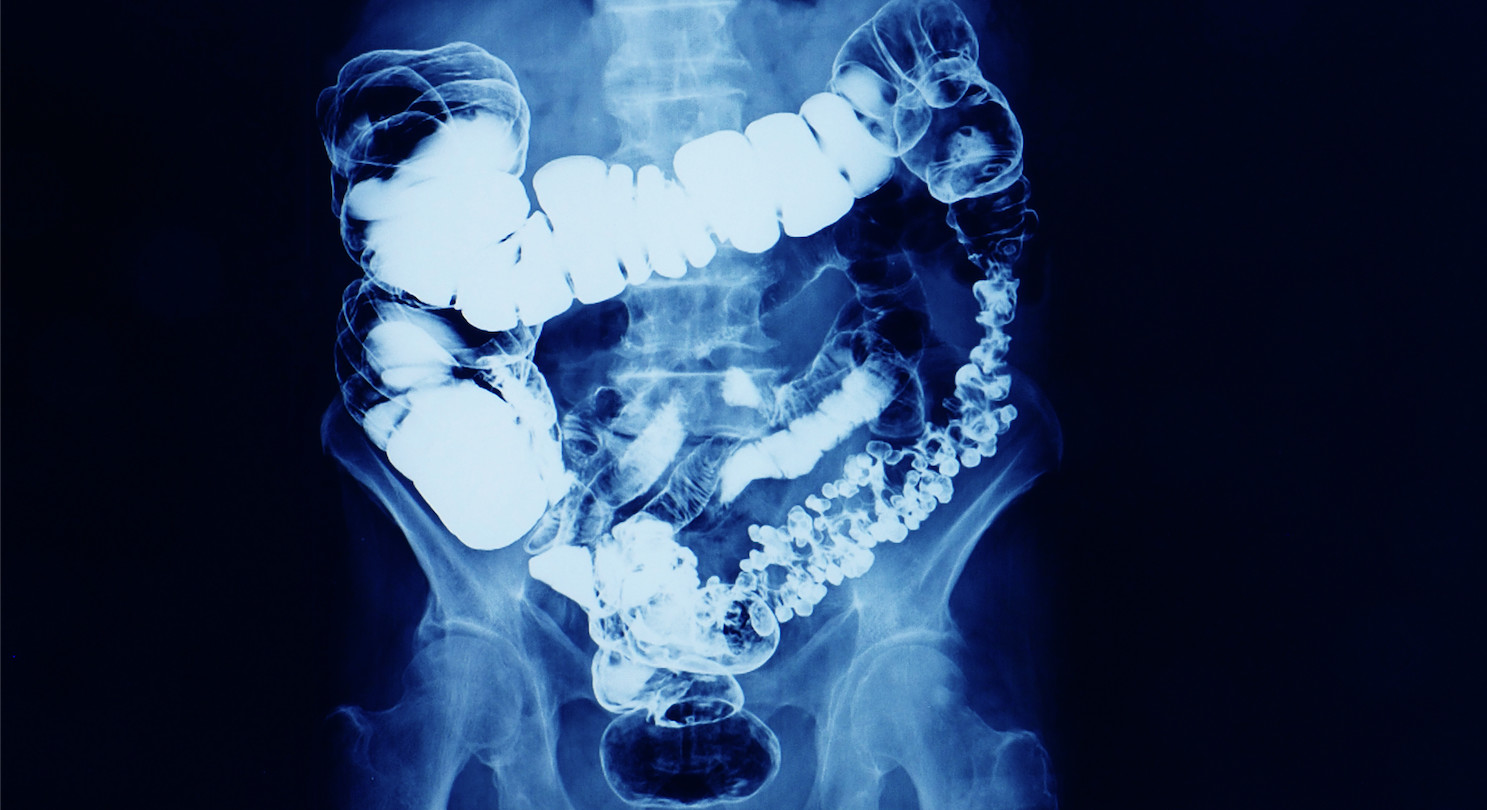
Bowel or colorectal cancer is Australia’s second most commonly diagnosed cancer in women and third most diagnosed in men. An estimated 15,500 people diagnosed with it in 2020.
It is our second most deadly cancer and expected to kill 5,300 Australians in 2020, which is more deaths than for breast cancer, prostate cancer or melanoma.

But these figures shouldn’t be this high because the majority of these bowel cancer deaths can be prevented. When caught early, the bowel cancer survival rate is over 95 per cent.
So, what can be done to save these thousands of lives?
Our research groups are taking a four-pronged approach to improve early detection of colorectal cancer through different approaches covering health services, public health, and laboratory research.

Health & Medicine
Rethinking gastrointestinal cancer diagnosis
People in Australia over the age of 50 should be familiar with the at-home poo-test kit.
The National Bowel Cancer Screening Program offers a free, safe, and accurate home test kit to Australians aged 50-74 every two years.
But each year, only 43 per cent of the 3.3 million people sent kits actually participate, meaning that almost two million Australians are declining this screening test.
Participation is even more dire for those first entering the program at age 50, with only 30 per cent of the 300,000 invited first-timers completing the test.
These people aren’t protected from preventable bowel cancer and are therefore unnecessarily vulnerable.

They either don’t prioritise the test, are ambivalent about doing it, or distrust it.
But much greater participation is achievable, so research in my team is embarking on a five-year program to increase bowel cancer screening participation by at least 20 per cent to save 25,000 lives and $A400 million in health care costs for cancer treatment.
Health & Medicine
A chip off the DNA block
Screening is the most effective strategy by far for preventing bowel cancer deaths, requiring less than an hour of your time every two years.
However, many people avoid the test for reasons including fear of diagnosis, the ‘yuck factor’ of collecting your own poo sample, or just not seeing it as a priority.
Our goal is to develop, trial, and cost new interventions to overcome the existing barriers to maximise participation.
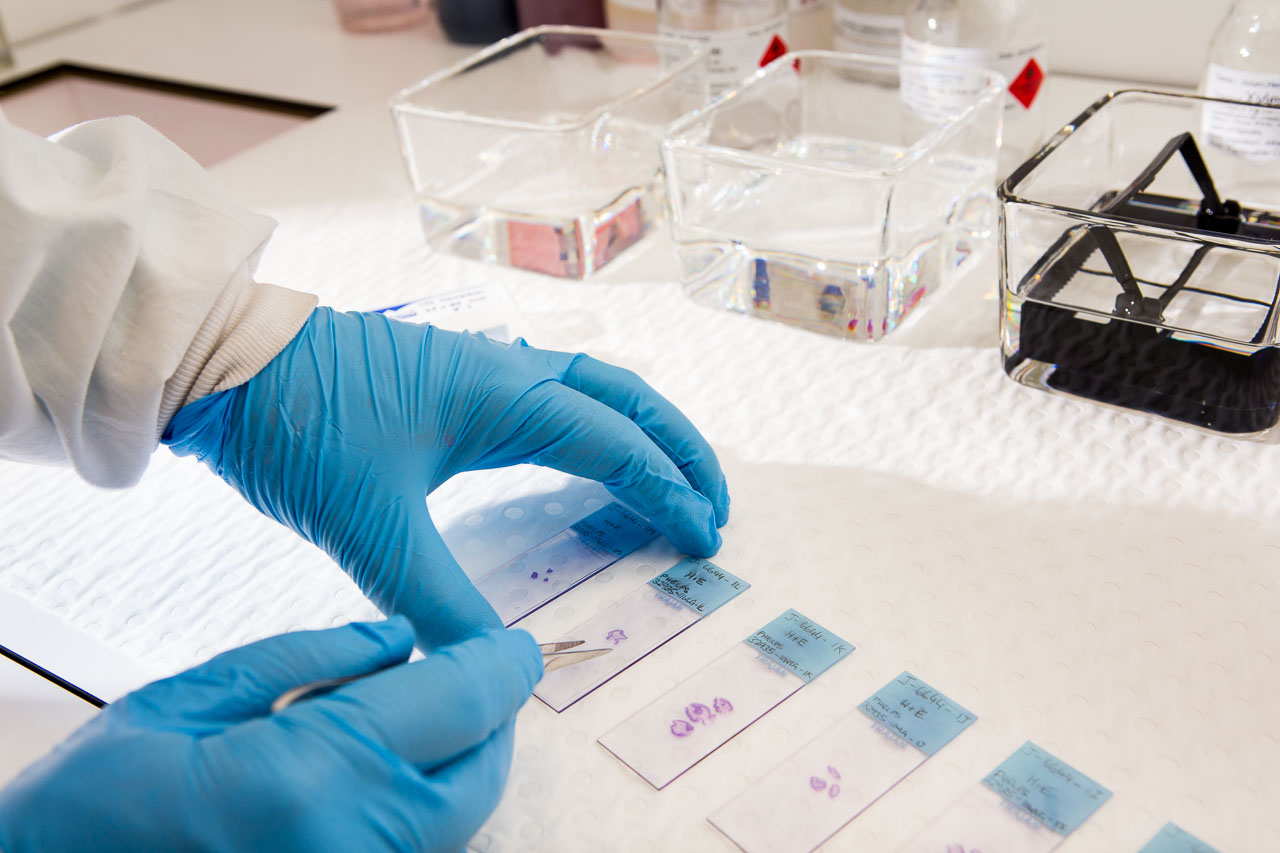
Doctors are often the first port of call for patients, so primary care is pivotal to improving early detection of bowel cancer.
GPs manage symptom assessment and ensure that patients receive appropriate cancer screening according to their risk of developing cancer. Even though we have a national bowel cancer screening program, the majority of patients are still diagnosed when they present to their GP with symptoms.

Professor Jon Emery’s research is identifying why diagnostic delay occurs in a primary care setting, to develop and test new diagnostic algorithms to prompt earlier investigation for cancer.
One of these is a decision support tool to assist GPs to better recognise patients at risk of an undiagnosed cancer, which is being developed as part of the Future Health Today research program.
Professor Emery is working to evaluate the use of genomic tests in primary care to identify individuals at increased risk of bowel cancer to inform tailored and more targeted screening.
Health & Medicine
The Global Cancer Atlas
Through applying these advances in cancer genomics and using technology to improve patient care, this work is transforming approaches to detect cancer earlier through a visit to your doctor.
Some people are at higher risk of colorectal cancer due to changes in their DNA or the development of pre-cancerous growths (polyps).
Being able to identify these risk factors and understand why colorectal cancer develops in people under 50 years old will allow us to prevent these cancers or catch them earlier.
Associate Professor Daniel Buchanan is leading a research program to identify people who have a high risk of colorectal cancer, and need intensive screening for early detection.

By using novel techniques to study multiple dimensions of the bowel, this work will provide a deeper understanding of high colorectal cancer risk settings.
These factors include the microbiome (all of the bacteria, fungi, and viruses that live in the bowel), the immune cells, types of pre-cancerous growths, and epigenetics – the changes that alter how DNA is ‘read’ by the cell.
By predicting who is at higher risk, early detection and treatment strategies can be targeted and personalised to those who need it most.

Health & Medicine
Is a delayed cancer diagnosis a consequence of COVID-19?
Early onset colorectal cancers – those diagnosed before the age of 50 – are increasing.
This is in stark contrast to the overall incidence of colorectal cancer cases, which have been consistently falling over the last 20 to 30 years.
Screening and early detection have been pivotal in effective prevention of the disease, however screening doesn’t cover people under the age of 50. As such, the majority of colorectal cancers in young adults are diagnosed at a late stage.
Associate Professor Aung Ko Win’s work will focus on enabling tailored prevention and detection for colorectal cancer in people under the age of 50.
His aim is to develop a risk-assessment tool to optimise screening, identify risk factors, and recruit the children of people with early onset colorectal cancer to develop future research.
By attacking bowel cancer from four angles our goal is to reach as many Australians as possible through these new programs of health services, public health and advances in laboratory research.
Together these approaches will provide the shake-up that’s needed to stop this prevalent cancer in its tracks, through both short- and longer-term approaches.
These four research projects are funded by National Health and Medical Research Council (NHMRC) Investigator Grants to improve cancer screening and outcomes.
Banner: Getty Images