Health & Medicine
Following cancer’s status updates
Australia’s world-class medical research has transformed cancer care, but patients may not see the benefits of new genetic testing without new funding models
Published 10 May 2022
The COVID-19 pandemic has put Australia’s health system in the spotlight for the past two years.
Much of that attention has been to ensure our health service has sufficient resources to manage the increased demand for people with severe coronavirus infection. But our latest adversary – the Sars-Cov2 virus – also impacts the timely diagnosis and treatment of other disabling or lethal conditions like cancer.

And as our population grows and ages, the number of people living with or beyond cancer is expected to increase by 72 per cent in the next 22 years.
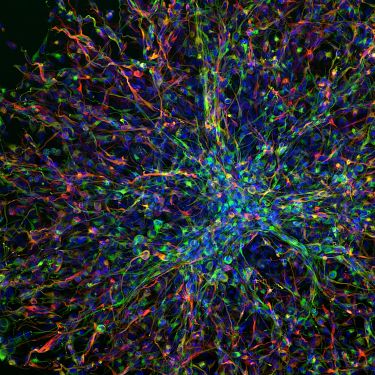
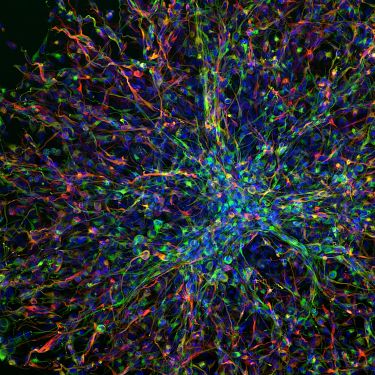
For every cancer, there are approximately five genetic changes that enable a tumour to increase its growth rate, move into nearby tissues and evade our immune system. So, discoveries in genomics will be critical to understanding and managing the disease.
Health & Medicine
Following cancer’s status updates
But how do we ensure our health system can incorporate these new genomic innovations when it already faces immense pressure to work with finite resources?
Compared to other universal health systems, Australia’s model is complicated with funding coming from state and federal governments as well as private health insurers.
New cancer drugs, medical devices and services are funded by either the Pharmaceutical Benefits Scheme (PBS) or the Medicare Benefits Schedule (MBS) based on expert advice on what treatments should be included or ‘listed’ on the PBS.
The listing of new treatments also has implications for state budgets, which explains why the cost is considered as part of the assessment process.
For cancer drugs, the system works well, with the PBS covering expenses. But it gets more complicated for some types of cancer testing, particularly diagnostics, which are molecular genomic tests that match a patient to a specific drug or therapy.

“MBS listing of companion diagnostics now follows the listing of the cancer drug on the PBS and is, therefore ‘reactive’,” says Professor Maarten IJzerman, Chair of Cancer Health Services Research in the Faculty of Medicine, Dentistry and Health Sciences at the University of Melbourne.
His team, leading the health economics platform at the University of Melbourne Centre for Cancer Research and The Advanced Genomics Collaboration, develops the evidence to support a more adaptable and flexible approach with the right incentives to facilitate research translation.

Health & Medicine
Is a delayed cancer diagnosis a consequence of COVID-19?
“For cancer patients to access specialised drugs, they need to be tested for specific DNA mutations. These are identified from a tumour biopsy, using a list of recommended tests,” Prof IJzerman explains.
“But as the current system is reactive, new drugs and tests are added each time.
So, for some patients, this could be very inefficient, and at some point, even be more costly,” he says.
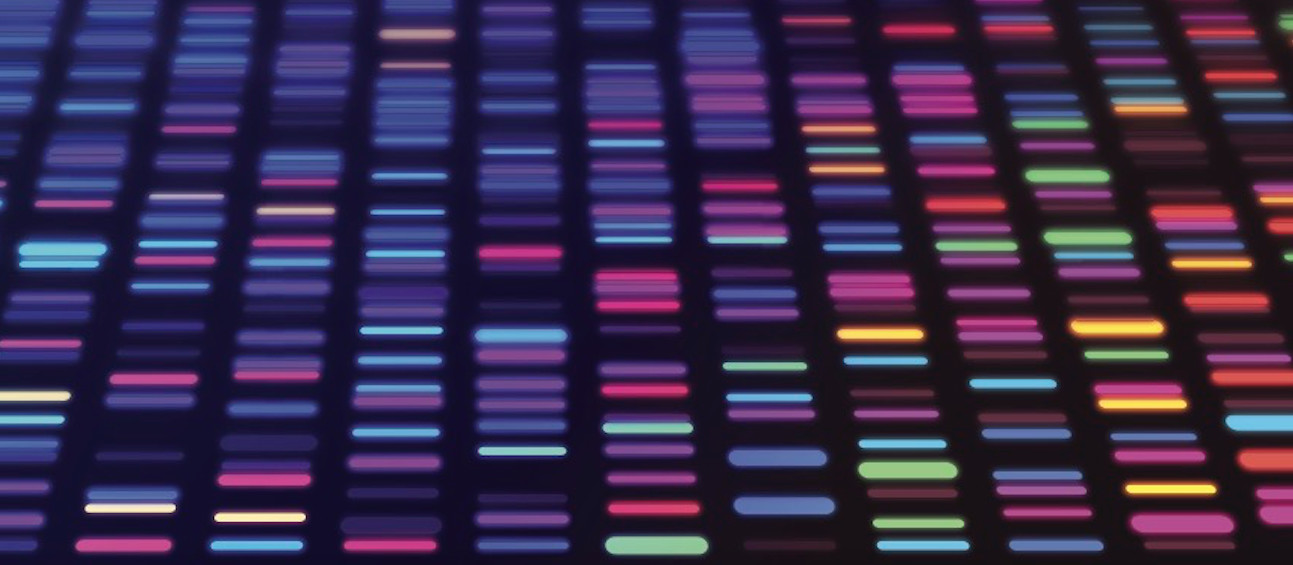
Using comprehensive gene panels – which test eligibility for several drugs at the same time – would make the diagnostic journey much more efficient. And this has rapidly evolved as the standard of care in most countries, including the UK and USA.
In several cases, even more advanced genomics technologies like Whole-Genome Sequencing (WGS) should be used to analyse the whole genome rather than a subset of genes. Cases that would particularly benefit from genome sequencing include rare cancers like Acute Lymphatic Leukemia or Cancers of Unknown Primary or CUP (where the original site of cancer growth is unknown).
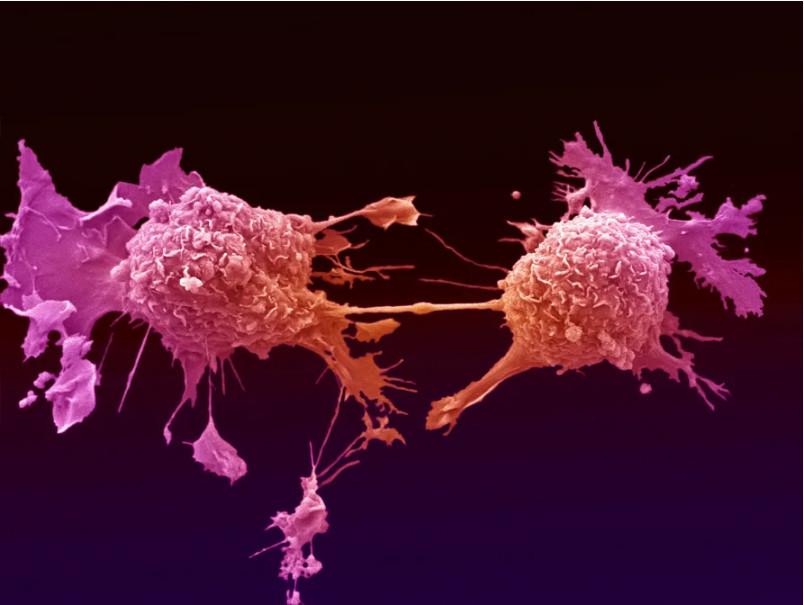
Cancers like CUP may have up 20 to different genetic mutations underlying their disease, so a doctor is currently required to provide the evidence for 20 different tests, making it harder to diagnose and design treatment in a timely way.
With WGS, clinicians can study DNA directly from a patient’s tumour and identify the genes, and DNA changes underlying their disease. This valuable information provides the life history of the cancer and reveals possible ways to personalise their treatment according to the specific DNA changes.

Health & Medicine
Our genetic strength in numbers
Prof IJzerman explains that the Netherlands government recently announced that around 1,500 patients with CUPS each year can access WGS, a decision which is largely based on the complex diagnostic pathways and the burden of disease from the condition. This decision will also facilitate further research and translation of results in routine care.
“With a strong emphasis in Australia on clinical and economic evidence before listing, this can be rather complicated as it could take years to develop this evidence,” he says. “Although I am not promoting technologies for which there isn’t enough evidence, there could be other mechanisms that would facilitate earlier access.”
“Obviously, we should be conscious of the increasing healthcare budget and the implications of listing new cancer treatments for the sustainability of the health system,” adds Prof IJzerman.
“So rather than listing new molecular tests in the MBS on a per-test basis, Medicare could also provide a bundled payment for genetic diagnostic testing. And the rebate should then be based on the diagnostic complexity.”

For example, for very complex diagnostic pathways like CUPs or some blood cancers, a high benefit fee would be available. Similarly, if only one test is performed to select treatment, a low benefit fee would be appropriate.
With this approach, the decision to use next-generation sequencing (NGS) methods, for what conditions and when (at diagnosis or in advanced disease only) should be done based on guidelines from professional societies using global evidentiary standards.

Health & Medicine
Better cancer treatments from better data analysis
The incentive for innovation is with the health professionals, while the cap on the benefit fee also ensures efficiency. And more importantly, the opportunity cost caused by delays in access to treatment can be reduced.
While a block funding mechanism would potentially facilitate access to molecular testing (and treatment), payment reforms could also drive research innovation and translation.
“Using new techniques like genomics in cancer care should also provide new investment and employment opportunities for Australians. The new technology provides the incentive for companies to invest in invention and innovation, driving employment and even export opportunities,” Prof IJzerman says.
For every decision to include a test on the MBS there will often be important clinical and economic arguments to reject, he explains, but we need to expedite the decision process to encourage companies to want to become part of the Australian industry.
“Waiting five years for a decision makes it more attractive to look overseas for an opportunity and take it to market,” he says.

And, while equitable access to care for all is a cornerstone in the Australian system, long delays in listing on the MBS will obviously benefit the wealthy who are able to pay out of pocket.
So, improving access to Medicare isn’t only a commercial interest, it’s also a societal responsibility striving for equity in access and outcomes.

Health & Medicine
Improving the care and wellbeing of cancer survivors
In Victoria, the University of Melbourne has recently partnered with Illumina, a leading international genomics company, with support from the Victorian government, to establish The Advanced Genomics Collaboration.
“It is extremely important to have an industry partner like Illumina to drive the higher-level vision of future cancer care,” Prof IJzerman says.
“With a different mindset and some risk-taking, we can bring in every option we have to make Australia a leader in cancer diagnosis and care.”
This research is part of The Advanced Genomics Collaboration (TAGC), a partnership between Illumina and the University of Melbourne to increase genomics innovation, its translation and adoption into the healthcare system and improve patient outcomes.
TAGC has three core platforms that enable research, analysis, trials and commercialisation: Clinical Genomics Platform, led by Professor Sean Grimmond; Bioinformatics Platform, led by Professor Oliver Hofmann; Health Economics Platform, led by Professor Maarten IJzerman.
Banner: Getty Images