Confessions of a professional baby maker
The science behind healthier embryos and better IVF
Published 14 July 2017
Reproductive biologist Professor David Gardner explains what we’re still learning about healthy embryo development, how it’s being applied to improve IVF technologies, and the unexpected insights it may offer into how cells implant themselves and proliferate - including how cancers take hold.
“Infertility affects one in six couples,” according to Professor Gardner. “I think people are often very surprised when they hear it’s that common.”
He adds: “I would love to see people thinking about having a family get the message that, before they come to a clinic, that they need to get fit. It’s ‘fit for fertility’ as it were, fit for reproduction, and look after themselves, because then you’re going to have healthier gametes which, in turn, you may not need IVF.”
Episode recorded: 22 June 2017
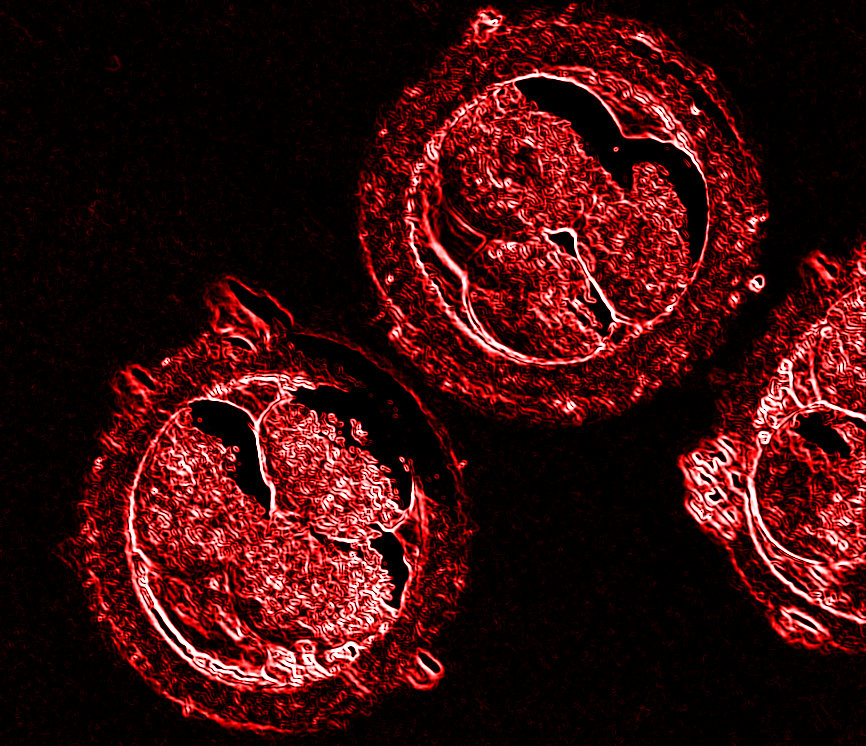
Up Close producer: Eric van Bemmel Audio engineer: Gavin Nebauer Banner image: Dr Elena Kontogianni/Wikimedia Commons
Subscribe to Up Close through iTunes.

