Health & Medicine
Curbing cancer’s addiction to treat it
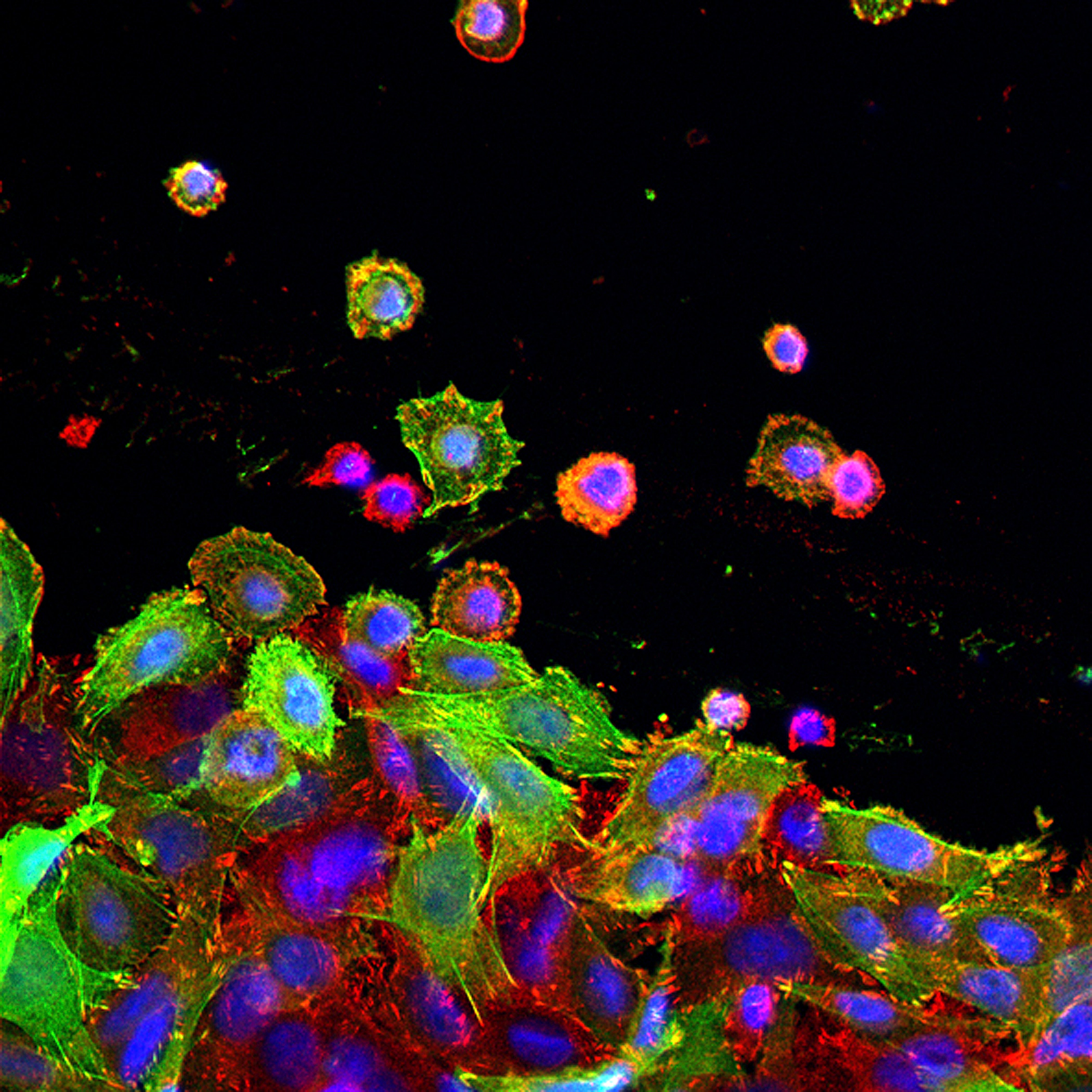
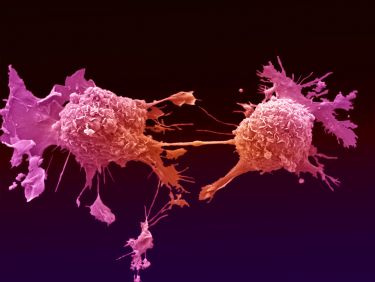
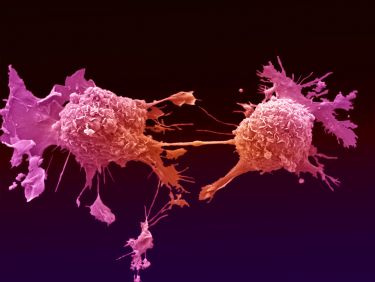
Professor Elizabeth Vincan’s research group were among the first to identify specific genes involved in an ancient form of cell-to-cell communication, and that if you could block them, it could provide a new way to treat cancer
Published 22 January 2020
Twenty years ago, Professor Elizabeth Vincan set out to understand how cancer cells ‘talk’ to each other and the cells around them.
Her research group was among a number to realise that some cancer cells always ‘switched on’ specific genes that function in an ancient form of cell-to-cell communication. And the idea was that if you could find out what these genes did, and block them, it could provide a new way to treat cancer.
Health & Medicine
Curbing cancer’s addiction to treat it
“At that time I was a young post doc mum and working where I was working was just too difficult because I had to go over the West Gate Bridge,” she says.
So when a position came up at Western Hospital that suited her, she fell into cancer research.
“The good thing about that is that I don’t actually have any formal cancer training, so when I address a question I come at it from a completely different tack. So that has been instrumental in the path that my career has taken,” Professor Vincan says.
“What I realised way back in the late 1990s is that growing – a solid tumour, for example, is very similar to growing an organ in the body. The same pathways are involved.”
Since then Professor Vincan, her lab and collaborators have been recognised for their work on cell to cell communication in cancer.
“We’ve shown that the genetic mutations that initiate cancer form the platform of disease. On top of that there’s the genes my lab work on, involved in a particular communication pathway. When we block a gene called Frizzled-7, we can actually hit cancer on the head,” she says.
Now, that to me is – has just been wonderful.”
Episode recorded: November 12, 2019.
Interviewer: Dr Andi Horvath.
Producer, editor and audio engineer: Chris Hatzis.
Co-producers: Silvi Vann-Wall and Dr Andi Horvath.
Image: Lorna McInroy/ Wellcome Trust