
Sciences & Technology
What’s behind gluten sensitivity when coeliac tests are negative?

We know the low FODMAP diet and cognitive behavioural therapy can both help Irritable Bowel Syndrome sufferers. But which one works best for whom?
Published 30 June 2025
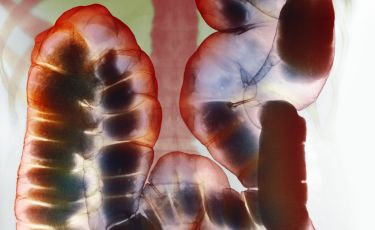
Irritable Bowel Syndrome (commonly known as IBS) affects around one in five Australians. It’s a chronic and often debilitating condition, with symptoms including abdominal pain, bloating, constipation, diarrhoea and unpredictable bowel movements.
The gold standard treatment in Australia – and internationally – is the low FODMAP diet, which restricts fermentable sugars found in foods like onions, garlic, apples, milk and wheat.

Statistically, it can be effective for around 75 per cent of people, helping to manage symptoms and improve their quality of life.
But what about the other 25 per cent? Our new clinical trial aims to work that out.
Our team’s recent six-month longitudinal study found that not all patients benefit equally from the low FODMAP diet.
In fact, psychological traits like gut-specific anxiety, personal control and perceptions of illness may play a key role in determining who benefits and who doesn’t.

Sciences & Technology
What’s behind gluten sensitivity when coeliac tests are negative?
That’s why we’re now launching a world-first international clinical trial comparing the low FODMAP diet with a very different approach: exposure-based cognitive behavioural therapy (CBT).
CBT helps people with IBS retrain how their brain responds to gut symptoms and feared foods, reducing anxiety and avoidance through gradual exposure.
The trial – an international collaboration between the University of Melbourne, Monash University, Harvard Medical School, Massachusetts General Hospital and Karolinska Institute in Stockholm – aims to recruit 200 people across Australia and the US.
These participants will then take part in 12 weeks of treatment entirely online from their own homes.

Unlike the low FODMAP diet, which works by avoiding trigger foods, CBT can help patients reduce fear and avoidance by gradually reintroducing those same foods.
Its aim is to reshape the gut-brain response through exposure exercises and psychological tools.
The gut and brain constantly talk to each other. In IBS, this communication can become oversensitive to normal signals from the gut. This can cause pain, bloating or changes in bowel habits.
Stress can make it worse. Understanding this helps guide treatments that can calm these signals and improve symptoms.

Health & Medicine
Making the most of probiotics
Both treatments are already in routine use and show similar success rates in clinical practice.
But until now, no one has directly compared them or identified what drives a person’s response to one over the other.
This randomised head-to-head trial – the first of its kind – will explore both the mechanisms (how the treatments work) and the moderators (who they work best for).
In doing so, it will help pave the way for more targeted and cost-effective treatment pathways.
Half of all Australians experience gut health problems at some point – with one in seven reporting distressing, chronic symptoms.

IBS alone accounts for a major portion of hospital presentations and healthcare costs, as many people with IBS spend years – and thousands of dollars – cycling through appointments, tests and treatments.
If we have a better understanding of which treatment works for which patient, it could dramatically reduce both the cost burden and amount of time to relief.
Our goal is simple: match the right person with the right treatment – the first time.
If you’ve been diagnosed with IBS, are aged over 18 and want to take part, you can join the trial from anywhere in Australia.
Sciences & Technology
Getting to know your microbiome better
Participants are randomly assigned to receive either the low FODMAP diet or CBT, with professional support from dietitians or psychologists throughout the trial.
Participation is free, and follow-ups continue for six months after the program ends to help us measure long-term outcomes.
The trial is based on our conceptual framework of the disease and our recent study on psychological predictors of response to the low FODMAP diet.
Living with IBS can seriously affect quality of life – whether it’s missing work, avoiding travel, or feeling anxious about simple everyday activities.
This trial offers an opportunity to not only access expert care but also help us better understand how to personalise treatment for others facing the same challenges.

If you’ve experienced IBS symptoms and want to contribute to research that could change future care, this is your chance. It’s only through high-quality research – with real people involved – that we can improve outcomes and give more people lasting relief.
IBS can be managed – and with your help, we’re aiming to make that pathway clearer for everyone.
If you’d like to express interest in the trial or find out more, visit: www.gutresearchstudy.com or contact: gut-research@unimelb.edu.au.