
Sciences & Technology
The danger of surveillance tech post COVID-19

A collaboration between multi-disciplinary experts has engineered a “ventilation hood” designed to protect healthcare workers from COVID-19. And it could go global
Published 24 August 2020
In January, there were fewer than 500 confirmed COVID-19 cases globally. In the space of no more than nine months, this number has risen to 20 million and counting.
Considering this extreme increase in case numbers we’ve had to rapidly evolve our understanding of how this virus spreads and ways to protect ourselves against it.

There is increasing evidence that the COVID-19 virus spreads through aerosolised particles expelled by infected people.
These aerosolised particles are droplets expelled through a person’s mouth when they’re speaking, coughing or even singing, but they have evaporated down to a very small size – less than a tenth the width of a human hair.
Such small particles can hang around in the air for hours and in indoor areas that have typical commercial or domestic ventilation systems, these particles can even accumulate in some spots around the room.

Sciences & Technology
The danger of surveillance tech post COVID-19
As our understanding of the virus progresses, so too does the debate around the use of masks and other protective gear to guard against the virus.
In many parts of the world (although Victoria in Australia currently excluded), the public has the freedom to choose whether to wear face coverings.
But one demographic does not have the luxury of choice and is in urgent need of protection through adaptive design: healthcare workers.
In a pandemic of infectious disease, the ability of frontline healthcare workers to continue working is paramount.
Healthcare workers around the world are falling ill at alarming rates and Australia is not immune, with thousands of infections in frontline staff.
The stress and anxiety caused by insufficient protection must be mitigated, because there are no helpful consequences to working under these conditions.
Moreover, no one should have to work in an environment that induces fear and anxiety; at least not without employers doing everything in their power to mitigate the risk.
Fantastic efforts in personal protective equipment (PPE), education, human resource management, systems efficiency, hospital engineering and many other processes have now been put in place to help.
But basic engineering solutions can help take away the risk at the hottest spot: the point at which healthcare workers are interacting directly with a patient.

Business & Economics
More transparency needed in PPE supply chains
Unfortunately, since we have never needed these solutions in the past, new ideas are needed, expert design is required and partnership with industry must be harnessed. And all of this has to happen at light speed.
Before all that, we need clinicians to reach out with a need.
Dr Forbes McGain, an intensive care specialist at Western Health, saw the degree of COVID-19 distress amongst his colleagues.
He had the idea to provide a sense of protection to his staff.
Imagining something that could maintain the highest standard of patient care while minimising infection risk, he contacted the University. That’s where Professor Jason Monty, head of Mechanical Engineering stepped in – developing a prototype personalised ventilation hood.

“Dr McGain revealed to us a serious unmet need in hospital response to the pandemic, which is to contain the COVID-19 virus expelled by patients in a hospital, in order to reduce the risk of infection for healthcare workers” Professor Monty says.
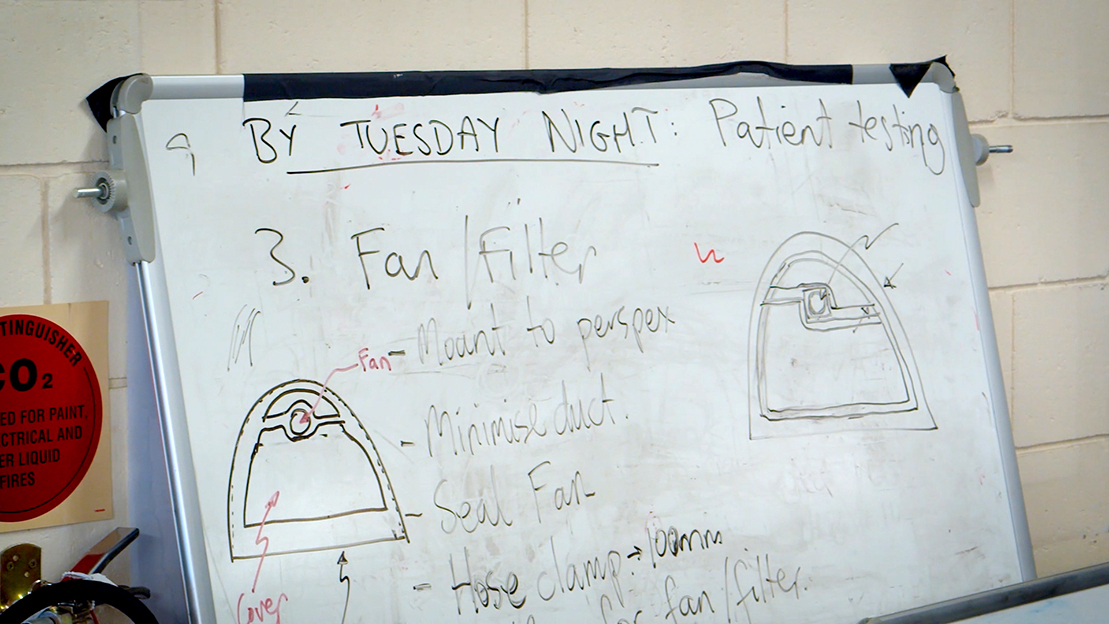
Working at speed, within 48 hours Professor Monty had designed a solution and assembled a team of engineers including Max Rounds, Dr Will Lee, Dr Kevin and Geoff Duke.
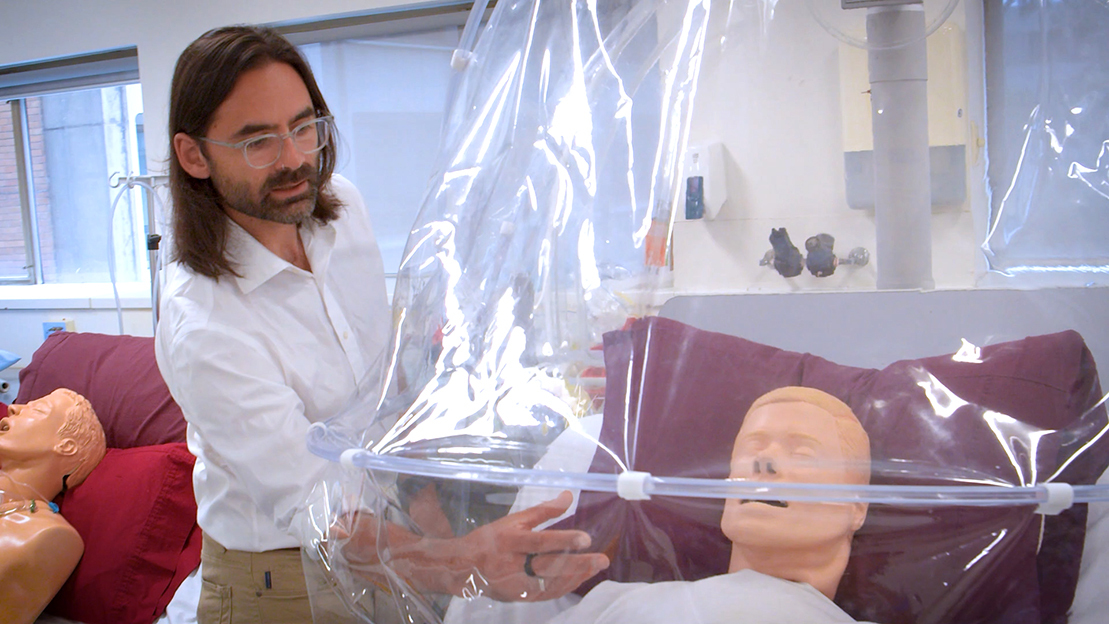
Together they built a PVC plastic fold-back ‘pram hood’ cover, they’re calling the personalised ventilation hood, which is designed to be installed behind a bed and cover the upper body of the patient.

Business & Economics
How are Australia’s doctors faring during COVID-19?
The cover provides a transparent barrier between the patient and the healthcare worker as a primary control of infection. As you can see through it, the hood also allows visual welfare checks and ease of communication between health staff and patient.
While other countries have explored methods such as Italy’s “bubble helmets” for critically ill patients in intensive care or the UK’s whole bed, sealed “isopods” (a rather morbid version of the Aussie “swag”), the personalised ventilation hood is designed with patient comfort and usability for healthcare workers as primary goals.
Most importantly, the hood is not airtight, preventing any risk of asphyxiation, while maintaining easy access for healthcare workers monitoring a patient’s vital signs.
That COVID-19 is an airborne disease has been debated around the world, but atmospheric chemist, Dr Robyn Schofield, notes that ‘pandemic respiratory aerosol specialists’, like Queensland scientist Professor Lidia Morawska, have consistently highlighted that ignoring airborne transmission of COVID-19 is risky.

And there’s now convincing evidence of outbreak clusters that are associated with indoor transmission.
PPE is the last line of risk mitigation, and the personal ventilation hood provides a physical barrier which reduces that higher level of risk.
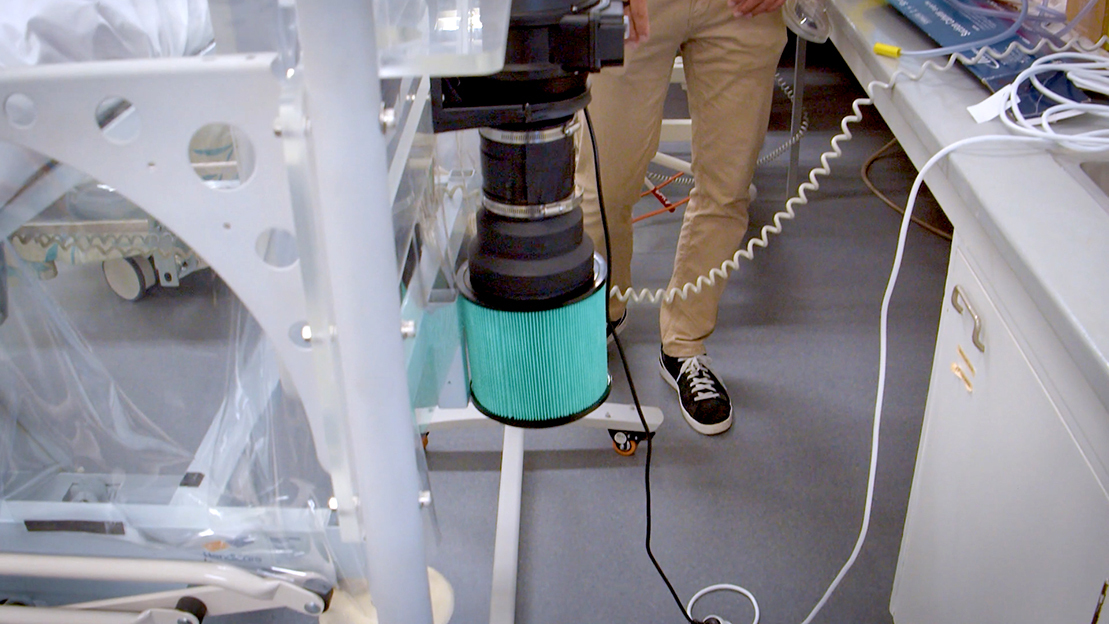
The high air flow within the hood prevents the aerosols and droplets produced from the patient’s breathing from coming out into the room.

Instead, the air within the hood flows through a duct above a patient’s head and particles that could potentially harbour the virus are trapped with a HEPA (high-efficiency particulate) filter that filters out 99.97 per cent of those particles from the air.
The design process – while quick – was not straightforward and followed embedded engineering design thinking of the crack research engineering team Professor Monty assembled.
The process has involved a clear statement of the design criteria, ideation, sketches, discussions, lengthy days and nights in the engineering workshop and constant consultation and feedback from ‘stakeholders’: the nurses and doctors who will eventually use the hood in ICU to protect themselves and other patients.
More importantly, the team aligned with a clear vision, so that all decisions could be made quickly in the build-up to the demonstration of the first prototype at Footscray Hospital.
Within 10 days of that first demonstration, the team built and tested two more prototypes, while local Australian manufacturers (Evan Evans and Westaflex) were contracted to produce hundreds of units per week.
“I was surprised to find that many local manufacturing companies and suppliers had capacity and were eager to help because their regular work was on hold as a result of the pandemic” Professor Monty says.

Health & Medicine
As a health worker, what’s my risk from COVID-19?
Clinical trials led by Dr McGain assessed the comfort for patients and usability of then hoods for staff at Western Health.
These trials have found a very high level of patient satisfaction and staff are satisfied with the hood’s extra protection. Clinical trials are now being rolled out to hospitals all around Victoria.
From here, the team are searching for a certified manufacturer to produce the hoods internationally.
Currently, the team is adapting an additional hood to fit to an ambulance bed, which would allow the safer transportation of COVID-19 patients and a reduced risk of exposure to emergency service workers.
The collaboration between multi-disciplinary experts including clinicians, mechanical and electrical engineers, atmospheric chemists, aerosol experts and industry lies at the heart of this success.
It also shows us that experts from diverse backgrounds and areas can come together in times of desperate need to produce engineering solutions that could potentially save lives and protect health workers.
Banner: Penny Stephens/Western Health