
Health & Medicine
Taking the ‘sex’ out of sexually transmissible infections
We know sexually transmitted infections like gonorrhoea are on the rise, and so is antibiotic resistance. If nothing else is available, would you accept the harsh treatments of the past?
Published 21 November 2019
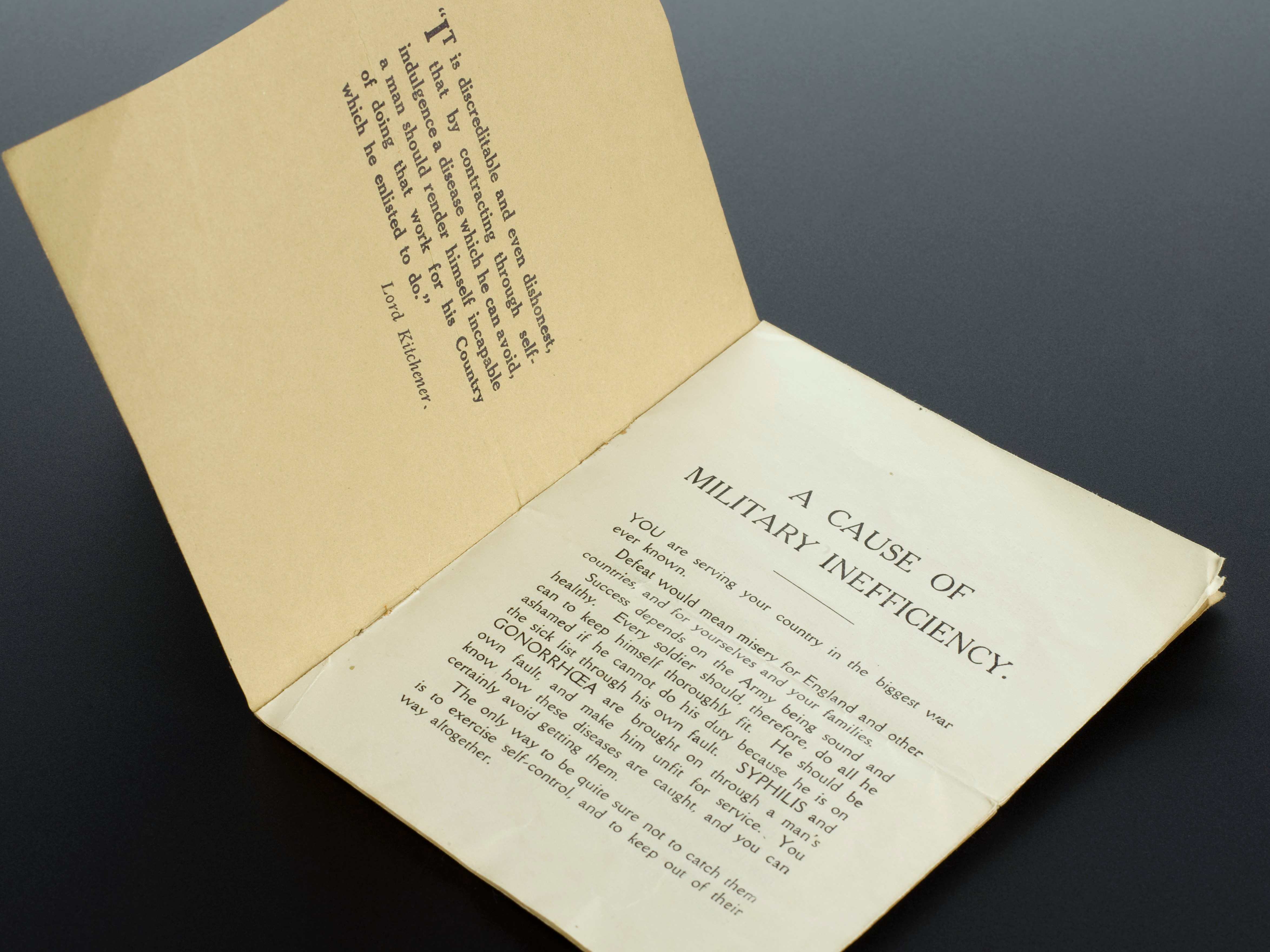
Gonorrhoea has a history of peaking around wartime when both risk taking and lust create a perfect storm of passion, but even without a war this sexually transmissible infection (STI) is on the rise.
So, should we be worried? Yes. Very.
A non-fatal infection that can cause inflammation of the genitals, rectum and throat, gonorrhoea was (until recently) easily treated by antibiotics. But the gonorrhoea bacteria is fast developing a high level of resistance to the two antibiotics used to treat it (ceftriaxone and azithromycin) as well as to all other antibiotics.
This strain of ‘superbug’ gonorrhoea has been reported in several countries including France, Japan and Spain, UK and here, in Australia.

Health & Medicine
Taking the ‘sex’ out of sexually transmissible infections
While, for many people, the infection will ultimately clear itself, the consequences of superbug gonorrhoea could be terrible, especially on a global scale – untreatable acute and chronic lower abdominal pain, increased infertility, miscarriages, maternal death due to ectopic pregnancy and neonatal eye infections that may cause blindness.
In mild infections, diagnosis can be easily missed.
Up to 80 per cent of women and 15 per cent of men with gonorrhoea have none of the obvious symptoms including genital pain, burning or discharge. They may continue to have unsafe sex and spread the infection.
What’s more, having gonorrhoea once doesn’t prevent you from getting it again.
The World Health Organization (WHO) has also predicted that untreated gonorrhoea will cause a five-fold increase of HIV transmission because HIV and gonorrhoea are associated with the same kinds of risk-taking behaviours.
In fact, an STI can make someone physically more vulnerable to acquiring HIV.

So, what next? If antibiotics are no longer effective, could we ever return to pre-antibiotic treatments?
Back then, the focus was on applying antiseptics to the urethra in men and the urethra and cervix in women. But the various ways of doing this were pretty brutal by today’s standards.

Health & Medicine
The birth of syphilis surveillance in Melbourne
From the 1920s, treatment commonly comprised ‘irrigation’ of these tissues over several days or weeks to wash out pus, and other debris of infection.
The male patient stood, wearing a waterproof apron through which his penis protruded, while a litre of fluid was held above his head and fed through rubber hosing inserted through the tip of the penis.
In acute cases, irrigation was limited to the first four to six centimetres of the urethra, using a cold solution to stimulate the sphincter to close off the rest of the urethral canal.
For chronic infection, the whole 18 to 22 centimetres of urethra from the penis to the bladder was irrigated. That meant using a warm solution to ensure the sphincter stayed relaxed.
These patients with a chronic infection lay down, and the fluid container was raised three meters or more in order to increase the gravitational effect and ensure the pressure was strong enough to reach the bladder.
Prostatic massage was performed before the irrigation was repeated.

But people who presented to the doctor with well-established infections required more aggressive treatment. For men, this might include careful insertion of instruments into the urethra to ‘release’ hidden bacteria and prevent strictures where inflammation narrows the urethral canal.
The Kollman dilator, with its umbrella-like activation was considered essential in chronic cases, known as ‘gleet’. Its description as an instrument of torture sounds justified, even if it was used with local anaesthetic.

Health & Medicine
We need to talk about chlamydia
Gonorrhoea also caused frequent complications.
Mr J. E. R. McDonough, who was a surgeon at the London Lock Hospitals, noted in 1915 that epididymitis – inflammation of the highly convoluted tube which carries semen from the testis – was extremely common.
Given the likelihood of sterility, it called for “special and energetic” treatment.
“Take the scrotum into one hand, make the skin tense over the epididymis and plunge a scalpel into its substance, in its long axis, in two or three places; the pain is momentary, but the relief which so quickly sets in is enormous.”
In women, clinical diagnosis relied upon visualising the discharge (pus).
Treatment focussed on applying antiseptics to the mucous membranes of the urethra (about four centimetres long in women), as well as to the vagina and cervix, up to four times a day. Organic silver compounds were also applied through suppositories or tampons.

More radical treatment for chronic infection involved destroying infected tissue by applying electromagnetic heat in a process called diathermy. Infected parts of the cervix could also be cauterised, or even destroyed by inserting a pencil of radium within the cervical canal.
In the mid-1920s to early 1930s, there was some success in treating gonorrhoea by heating the genitals.
Heat treatment was given at the US Mayo Clinic in a fever cabinet which left only the head exposed. The temperature was raised to 41°C for four to six hours, every three days over a period of five or six treatments.

Health & Medicine
Why is no-one talking about safe sex for the over 60s?
As an adjunct to this treatment, an element heated to 44°C could be inserted into the vagina and/or the rectum for up to two hours.
Whatever the treatment, US army data from 1937 shows that in the three years prior to the introduction of the sulphanilamide antibiotic, gonorrhoea typically required patients to be hospitalised for over 50 days, and 28 per cent developed complications.
But by 1941, antibiotics had reduced the average time in hospital to only 22 days, and complications has fallen to 6just six per cent.
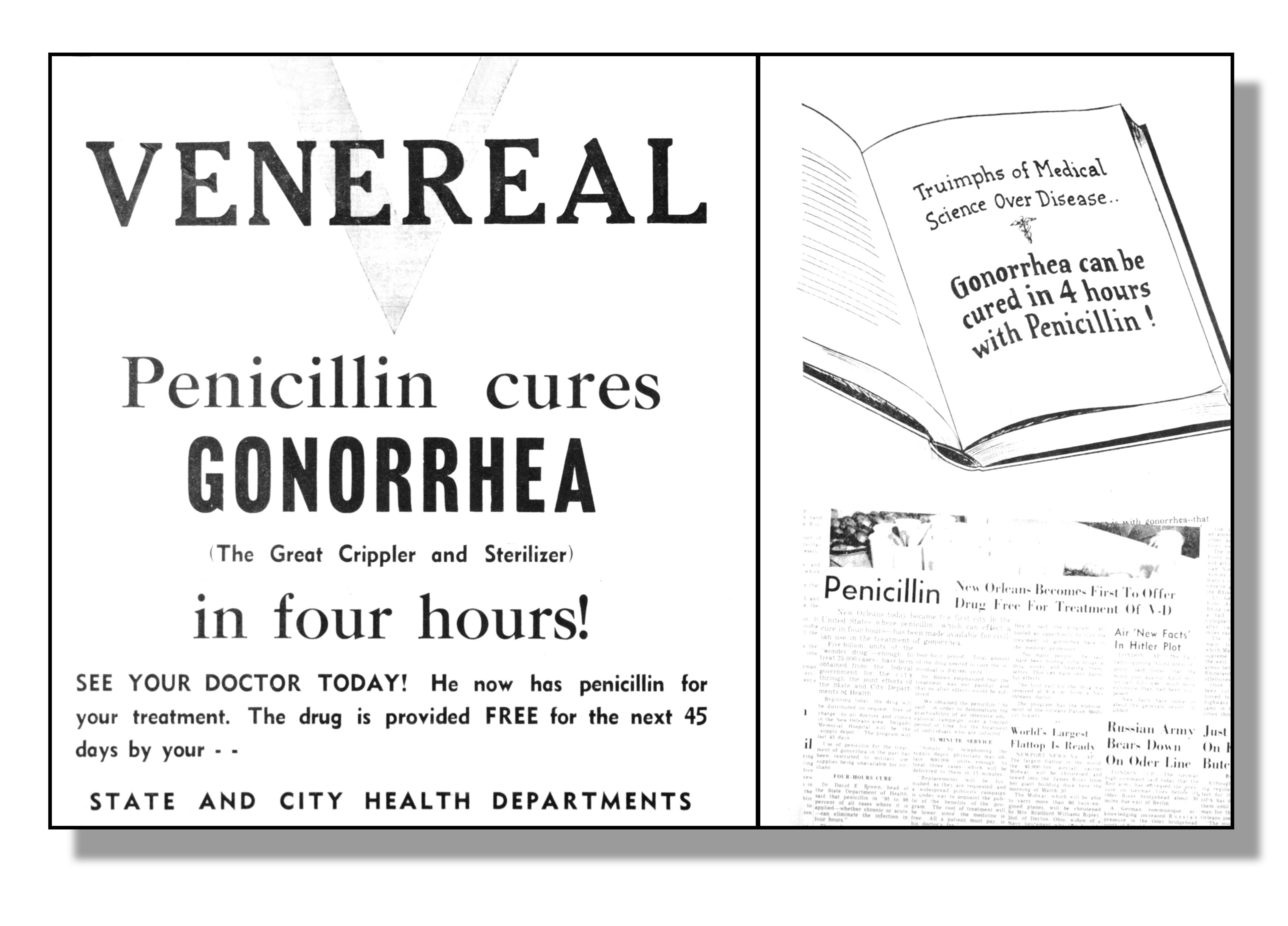
In the early 1940s, penicillin began to be used in patients in whom sulfa-based antibiotics had failed.
But, the bacteria was quick to adapt and even though doses were small, by 1946 penicillin-resistant infections were already being identified.
The number of resistant strains increased over the next 20 years and gonorrhoea bacteria have now gone on to develop resistance to almost every other suitable antibiotic.
There is, nevertheless, some hope for the future.
Recently, a mass vaccine campaign in New Zealand demonstrated that meningococcal B vaccine induces antibodies which also recognise gonorrhoea, offering a starting point for vaccine development.
But what can be done in the meantime?
The WHO has highlighted that changing behaviour is critical to reducing the spread of infection. We can’t rely on antibiotics or the development of new medicine, but we can reduce the likelihood of transmission by simple things like hand-washing and practising safe sex.

Health & Medicine
Lifting the lid on HIV
Recent evidence suggests saliva, when used as a lubricant in sex, can transmit gonorrhoea from the pharynx to the genitals, mouth or anus, but that mouthwash can lower this transmission.
One way to keep gonorrhoea bacteria under control right now is to make sure that people using antibiotics take the entire prescribed course, not just until symptoms have improved.
Also critical is sexual abstinence for seven days after treatment commences, and no sexual contact with previous sexual contacts from the last two months, until they have been tested and treated too.
When asked about why they had sex with a new partner without protection, it’s not uncommon to hear people say that they trusted their partner to be free of an STI.
Given that STIs sometimes show no symptoms at all, this is a fool’s game. It’s also the kind of statement that might lead to infection with gonorrhoea. Let’s hope it’s not the superbug strain.
This work was conducted during Professor Meredith Temple-Smith’s residency at Fondation Brocher in Switzerland.
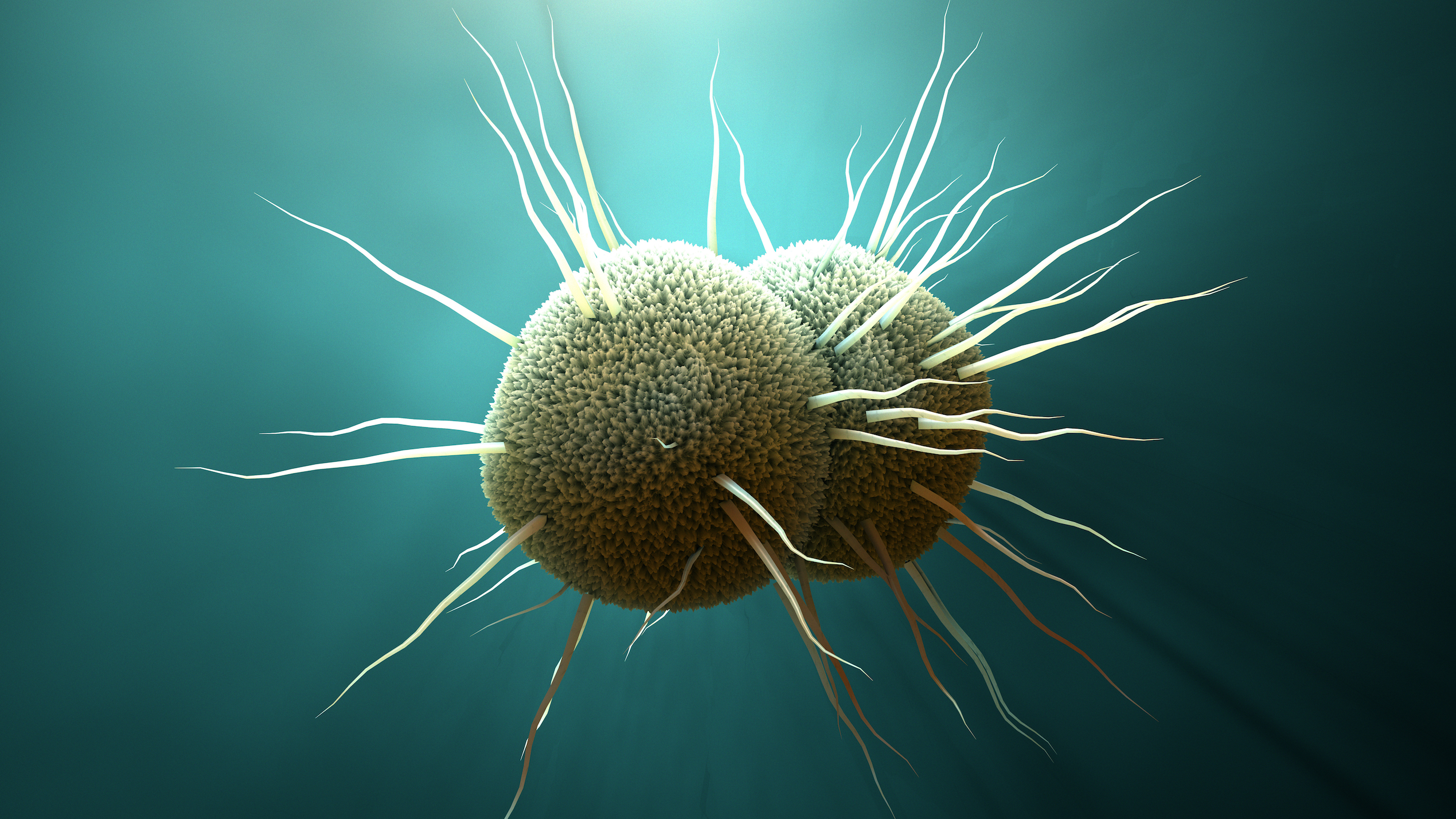
Banner: Neisseria gonorrhoeae bacteria/Shutterstock