
Health & Medicine
Targeting ovarian cancer

New research shows many Australian women mistakenly believe that ovarian cancer can be prevented through vaccination – telling us more needs to be done to raise awareness
Published 31 August 2020
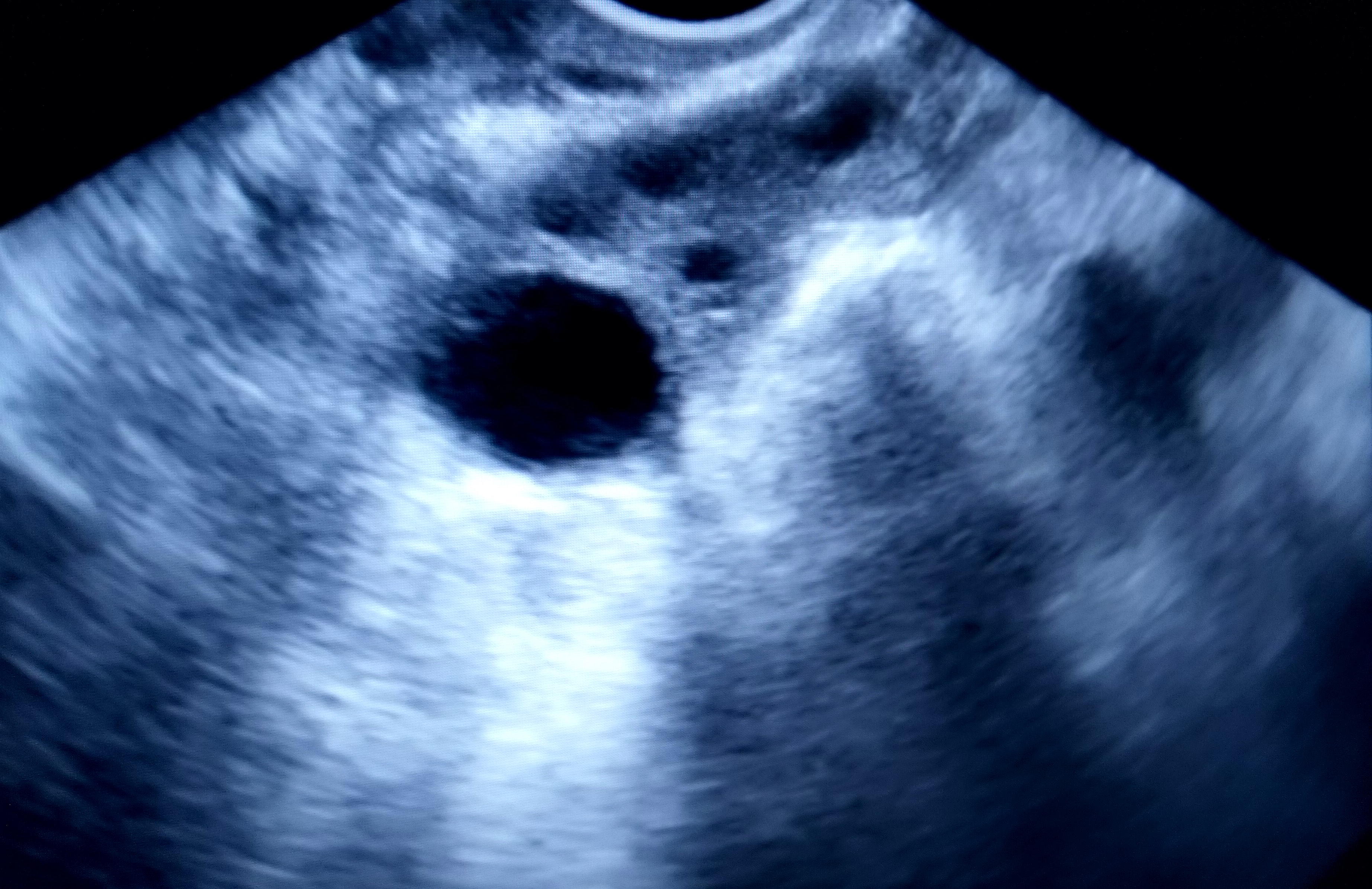
Ovarian cancer is diagnosed in almost 2,000 Australian women every year and it has the lowest survival rate of all the gynaecological cancers.
Unlike with cervical cancer, there is no vaccine to protect against developing ovarian cancer. Nor is there an early detection test.
But research by the University of Melbourne and the Ovarian Cancer Research Foundation has found that many women mistakenly believe that vaccines and early detection tests are available to prevent and manage ovarian cancer.
These misconceptions present significant challenges for women who are diagnosed with the disease.
The indeterminate nature of its symptoms is one of the most pernicious aspects of ovarian cancer.

Health & Medicine
Targeting ovarian cancer
Many of the warning signs – like abdominal pain or pressure, sudden abdominal swelling, weight gain or bloating, unexplained weight loss, low backache or cramps, and unusual feelings of fullness, gas, nausea or indigestion – can be easily dismissed or misinterpreted as a symptom of something less serious.
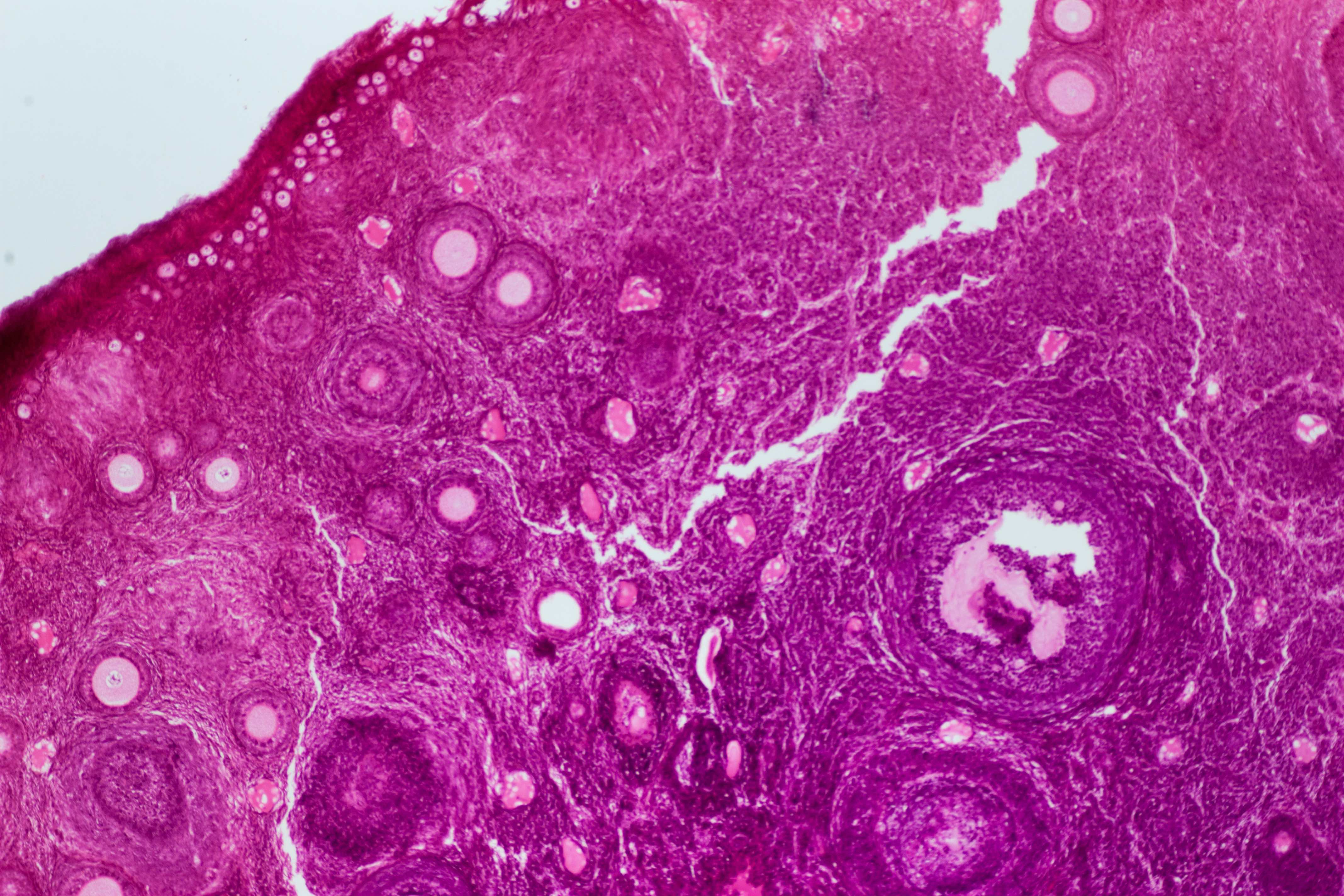
Additionally, the causes of ovarian cancer are also poorly understood.
Only 15 to 20 per cent of cases can be linked to specific gene mutations and there is no known cause for the remainder of cases.
In conjunction with its vague symptoms, the lack of any early detection test for ovarian cancer means that the majority of cases are only diagnosed once the cancer has reached its most advanced stage – when prospects for recovery and long-term survival are lowest.
The absence of an early detection test places the onus on women to be alert to the possible signs, vigilant in pursuing them with their doctors and undergoing multiple invasive steps to diagnosis.
A survey of 494 Australian women conducted in 2020 by the University of Melbourne and the Ovarian Cancer Research Foundation found that while recognition of this particular cancer is high – 95 per cent of women are aware – many women have poor understanding of the disease.
Health & Medicine
The blood test tracking down microscopic cancer DNA
Of greatest concern is the prevalence of misconceptions around prevention and detection:
68 per cent of women believe a cervical test can detect ovarian cancer – it can’t
65 per cent of women believe there is an early detection test for ovarian cancer – there isn’t
64 per cent of women believe a PAP test can detect ovarian cancer – it can’t
50 per cent of women believe the Human Papilloma Virus (HPV) vaccine protects against ovarian cancer – it doesn’t.
This misconception may be related to the fact that the HPV vaccine does protect against cervical cancer. Accurate understanding of the make-up of the female gynaecological system may also be a barrier to understanding the risks of ovarian cancer.

All of these misconceptions create risks if women are mistakenly relying on regular health checks to alert them to this serious health issue. Women may also become less alert to possible warning signals of ovarian cancer.
While women of all ages are generally consistent in their level of knowledge and understanding of ovarian cancer, there are suggestions that women under the age of 30 may be less aware.
Health & Medicine
Filling in the genetic blanks of breast cancer predisposition
Only 86 per cent of women in this age group indicate awareness of ovarian cancer in general, and 75 per cent believe that a cervical test or PAP test can detect ovarian cancer.
Although research is ongoing, neither a vaccine, an early detection test, nor a cure, are likely to be available in the near future.
So, to protect Australian women from the worst of ovarian cancer, the focus needs to be on increasing awareness of the existence of ovarian cancer and the importance of women looking for signs of the disease themselves.
According to Lucinda Nolan, CEO of Ovarian Cancer Research Foundation, this year, more than 1,800 Australian women will be diagnosed with ovarian cancer, and that by 2025, only 830 of these women will still be alive.

We still don’t have any way to detect ovarian cancer early, so it is imperative that women are aware of any symptoms that may suggest something is not right. Women know their bodies best, and they need to act on any concerns.
The Foundation is continuing its search for an early detection test because this would improve five-year survivability rates from the current 46 per cent, to more than of 90 per cent.
That is what all women deserve.
The research was an online survey conducted by the University of Melbourne and the Ovarian Cancer Research Foundation between 17 April and 24 April 2020, among a nationally representative sample of 494 women aged 18 years and older. The research was conducted as part of the Master of Applied Psychology industry partnership research project (by students Anh Tran, Sheng Shao, Yiwei Feng, Priya Ramkrishnan, supervised by Dr Isla Carboon).
Banner: Shutterstock