
Health & Medicine
The right antibiotic at the right time

As we mark Antimicrobial Awareness week, one Australian collaboration has been pioneering software solutions and research into antimicrobial stewardship for nearly two decades
Published 17 November 2021
Globally, success stories of software technologies enabling large-scale antimicrobial stewardship (AMS) are rare.
There are even fewer cases of tools developed by academics and clinicians working with software engineers in a single team to provide ongoing AMS innovations and academic research.
But a pioneering team made up of the University of Melbourne’s National Centre for Antimicrobial Stewardship (NCAS) and the Royal Melbourne Hospital’s Guidance Group, has become a multidisciplinary collaboration working on clinical and technological solutions for antimicrobial stewardship.
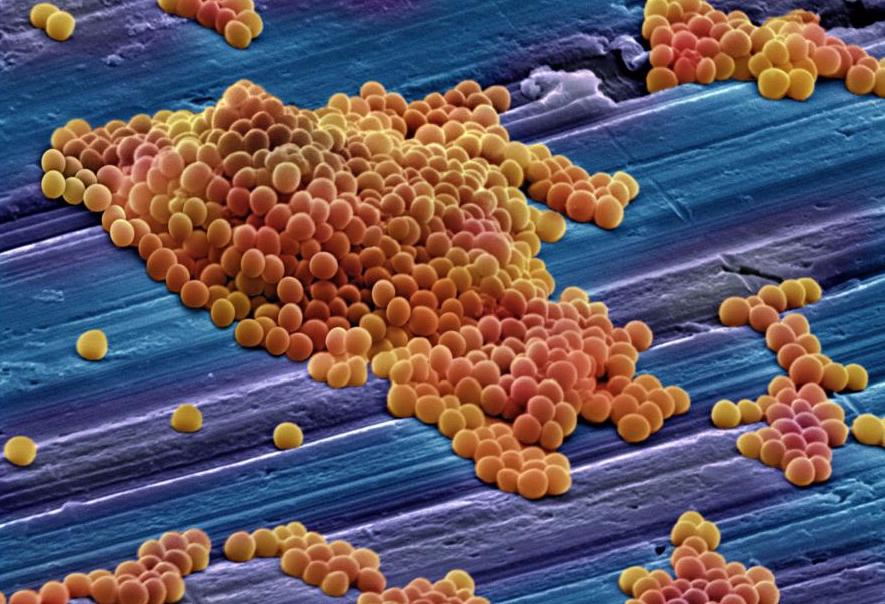
According to the World Health Organisation, antimicrobials – including antibiotics (like penicillin and tetracycline) antivirals, antifungals and antiparasitics – are medicines that are used to prevent and treat infections in humans, animals and plants.

Health & Medicine
The right antibiotic at the right time
But the inappropriate use of antimicrobials is closely linked with the emergence of antimicrobial-resistant bacteria.
At its core, antimicrobial stewardship aims to improve the appropriate use of antibiotics and reduce antibiotic resistance.
As leading infectious disease physicians and clinician-researchers, Professor Karin Thursky and Professor Kirsty Buising initiated two award-winning not-for-profit tools, long before stewardship existed on any meaningful level globally and in Australia.
Their aim is to assist clinicians to make the right antimicrobial choices and help hospitals to achieve their stewardship goals.
Guidance MS is an AMS decision support system that was launched in 2005 and is now used in over 60 Australian hospitals. While the National Antimicrobial Prescribing Survey (NAPS) is an auditing platform that is a key component of the Australian National Antimicrobial Resistance Strategy – now being implemented internationally.

“It’s very unique that we’ve been able to co-develop and co-design digital AMS solutions that have been scaled effectively and delivered data into the national system,” says Professor Karin Thursky, the director of NCAS, the Guidance Group and one of the original founders of Guidance MS.
The journey for the team started nearly 21 years ago when Professor Thursky, then an infectious diseases registrar at the Royal Melbourne Hospital (RMH), came across a 1998 article from the LDS Hospital in Salt Lake City, Utah.

Health & Medicine
Antibiotic use too long in surgery
The article described a decision support system for antimicrobial prescribing in the hospital’s intensive care unit (ICU) and was regarded as the potential “Holy Grail” of decision support systems, says Professor Thursky.
However, like so many ‘home-grown’ software systems at the time, it was not transferrable to any other hospital.
This sparked a lifelong interest in computerised decision support systems.
Professor Raina MacIntyre, who was the head of epidemiology in the Victorian Infectious Diseases Service at the time, and Professor Thursky applied for a grant from the Victorian Health Department, which funded the initial decision-support software, Advise. Developed and implemented in the Royal Melbourne Hospital’s ICU, Advise not only led to a reduction in antimicrobial use but also a reduction in the burden of resistant pathogens.
The project established the core team including Professor Kirsty Buising, who was then a registrar, that went on to build the antimicrobial stewardship program, now known as Guidance MS.
In doing so, the Guidance Group became one of the few teams run by academics and clinicians to build an on-the-ground digital solution for antimicrobial stewardship amid increasing global concern about the impact of antimicrobial resistance on infectious diseases care.
“Guidance came on the journey of AMS evolving in Australia,” says Professor Buising. “For a lot of the younger infectious diseases physicians and clinicians coming through, they sometimes don’t realise that stewardship essentially didn’t exist fifteen to twenty years ago.
“Our group and other stewards were responsible for developing the argument for why it needed to exist. We then imagined and devised what ideal stewardship systems should look like.”

Sciences & Technology
The tiny drop fighting the big problem of antibiotic resistance
Working alongside a dedicated team of software engineers meant the Guidance Group could design a transferrable, flexible system that supported the full range of hospital clinicians.
The team itself is made up of senior infectious disease physicians, microbiologists and specialised infectious diseases pharmacists.
“Different levels of clinicians have completely different requirements [from stewardship systems],” says Renu Padhmanaban, the head of technical services and one of the original software developers of Guidance MS.

“Working with clinicians, who are the end-users themselves, means we can integrate all these needs and deliver a simple solution.”
Professor Thursky says Guidance MS provides clinicians with the national prescribing recommendations for antimicrobials at the point of care and triages patients who may need review by stewardship teams.
“If you think about a 500-bed hospital where around 40 per cent of patients are on an antibiotic, there’s no way with current funding levels that the stewardship services can see all those patients without a support system,” she says.

Health & Medicine
Stronger action to curb overuse of antibiotics
As Guidance MS was rolled out in selected hospitals, the team were also able to provide a 360-degree execution strategy that supported hospitals to set up their own stewardship programs.
Independent research on the system has found results such as an increase in the appropriateness of prescribing, time-saving efficiencies, a reduction in antimicrobial drug expenditure, as well a proven reduction in resistance and infection levels.
In partnership with the Australian Government Department of Health, the NAPS has been adopted nationally as part of the national Antimicrobial Resistance and Usage surveillance program.
Now, it’s being used in Canada and New Zealand, as well as being piloted in hospitals in Malaysia, Papua New Guinea, the United Kingdom, Bhutan, Nepal, Vietnam, Fiji and Timor-Leste.

The NCAS animal health stewardship team led by Professor Glenn Browning and his team from the University of Melbourne’s School of Veterinary and Agriculture Sciences is also exploring digital solutions such as natural language processing and machine learning to drive antimicrobial stewardship.
Meanwhile, Guidance MS is also being completely redesigned with the ability to better integrate with electronic medical records in many hospitals, nationally. The system is also being used to support a virtual AMS model in rural and regional hospitals – like Goulburn Valley Health in rural Victoria.
Health & Medicine
The dark side of electronic medical records
“There’s a huge amount of disparity in healthcare across Australia, partly because of the geographical challenges,” says Professor Thursky.
It has continued to adapt to the needs of AMS programs, especially the requirement for effective auditing and feedback.
Meanwhile, the NAPS program provides a rich source of data that informs current hospital, jurisdictional and national strategies.
As a result of this team and their robust large-scale research that flowed from the practical application, Australia is now globally recognised for its systemic efforts to improve antimicrobial prescribing across the nation’s healthcare system.
Banner: Getty Images