
Health & Medicine
Chronic fatigue syndrome a kick in the guts
The ecological community your body’s hosting and its impact on your health
Published 1 September 2015
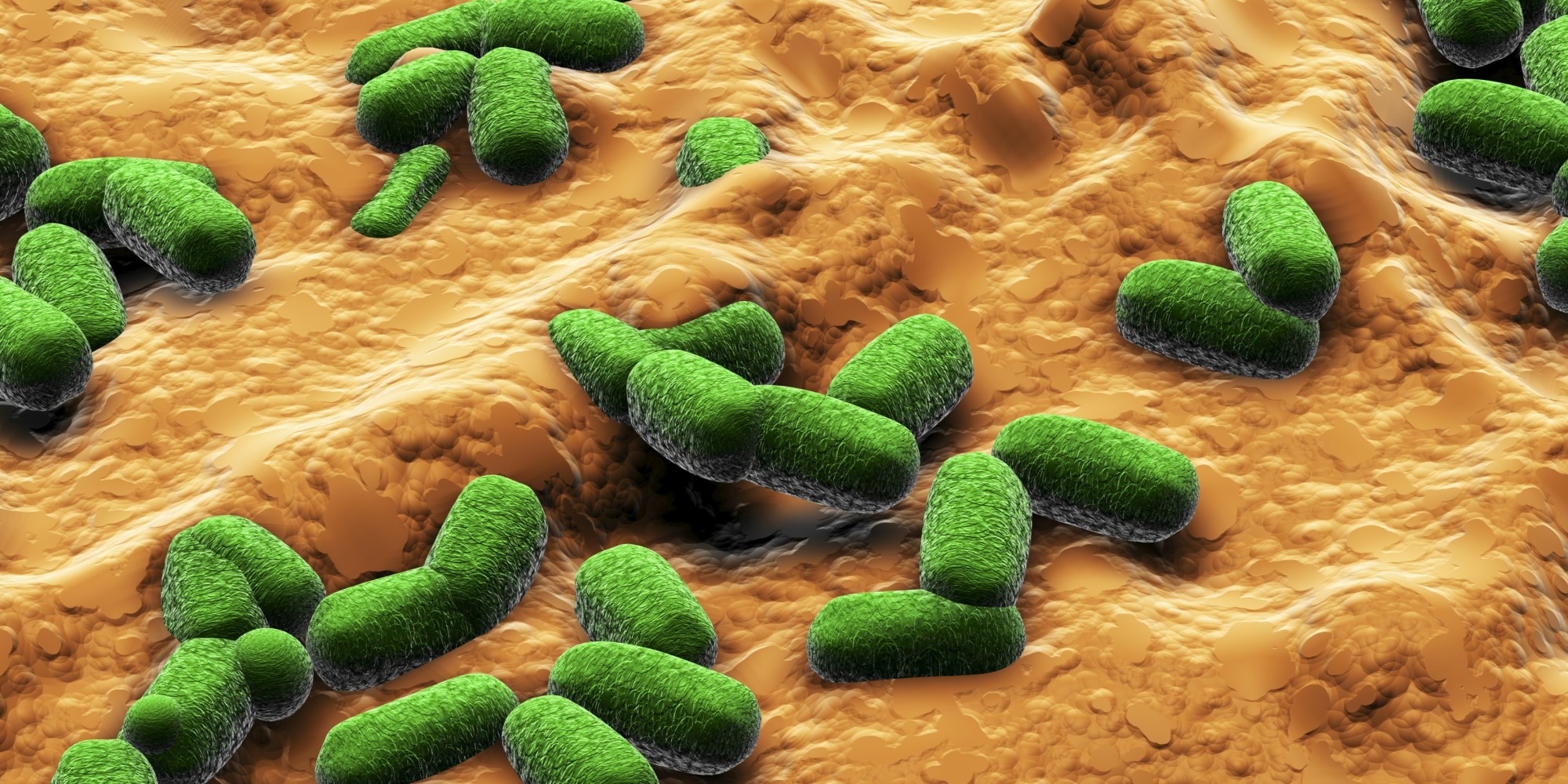
The Up Close podcast hears from chemistry researcher Professor Spencer Williams on the rapidly emerging understanding of human microbiota – the diverse and numerous microorganisms that reside on and within our bodies – and particularly how the composition of our gut flora can determine the state of our own health.
“There’s a strong correlation between diseased states and the composition of your microbiota,” he says.

Health & Medicine
Chronic fatigue syndrome a kick in the guts
“So a big question has been is this just coincidental or is there a cause? Is there change in the composition of your microbiome somehow causing these diseases? Increasingly the answer for some of these diseases appears to be yes.”
Subscribe to Up Close through iTunes.