
Health & Medicine
Hope in the darkness

New palliative care training for Sister Doctors in India is supporting patients and families during the pandemic and broadening understanding of care across the Indian Ocean
Published 18 November 2021
Many of us watched in horror and with great sadness as COVID-19 swept India earlier this year.
While our borders and our public health measures meant we had little COVID-19 infection in our community at that time, in India we saw nightly footage of people struggling to breathe, of others treated on the street and of families desperately seeking help for the person they loved.

Many of us have friends, colleagues and family in India, and felt helpless as we witnessed the suffering. However, as the peak of the wave passed, an opportunity, albeit small, to do something more tangible was realised.

Health & Medicine
Hope in the darkness
For the last few years, Palliative Care physicians and academics at Melbourne University and St Vincent’s Hospital’s Centre for Palliative Care have developed relations with Catholic Health Association of India (CHAI).
Beginning in 2018 with a visit to the CHAI headquarters in Hyderabad to develop relationships, conduct face-to-face teaching and begin discussions about a palliative care strategy, this relationship builds upon much older, deeper links.
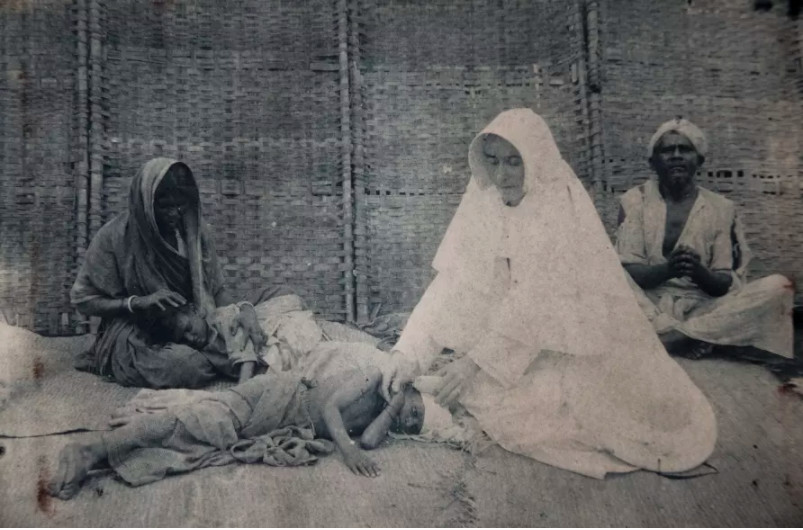
Indeed, these links were originally forged in the first part of last century through the work of Sister Doctor Mary Glowrey who grew up in country Victoria, trained as a doctor at the University of Melbourne and, following her deep commitment to the health of underprivileged women and children, became a medical missionary in India.
Mary’s approach to public health has many contemporary resonances today as she sought to develop sustainable systems for health care delivery to the poor.
It was Mary who established CHAI, which is now a network of 3,518 member institutions, including primary, secondary and tertiary care centres, medical and nursing colleges and social service organisations as well as over a thousand sister-doctors across India.

Health & Medicine
The woman who changed the lives of millions
Professor Nathan Grills, from the Nossal Institute for Global Health, has worked with CHAI over some years in the areas of HIV, disability and community development.
With the support of the University’s Faculty of Medicine, Dentistry and Health Sciences and St Vincent’s Hospital he led the establishment of the Sister Mary Glowrey Scholars scheme to support capacity building for staff at CHAI.
Under this program, the Centre for Palliative Care at the University of Melbourne formed a productive relationship to deliver collaborative teaching and strategic service development. It is from this background that in the time of COVID-19, the opportunity to deepen these relationships emerged.
In response, our team recruited a number of leading Australian and Indian palliative care physicians to work with CHAI is delivering an online course – ‘Palliative care in the era of COVID-19’ to 67 Sister Doctors, who are both nuns and physicians, and work in a variety of settings from large metropolitan hospitals to community clinics servicing tribal areas.

For two evenings a week for four weeks, the group worked through approaches to symptom management, decision making and triage of patients, difficult conversations and bereavement care, and managed to create a space for interactive learning through discussion and conversation.

Health & Medicine
How one misconception means seriously ill people miss out on care
The Sister Doctors presented cases of encounters they have had in their practice, seeking input from the faculty and their peers, and prompting wide-ranging discussions.
The cases and discussions weren’t limited to COVID-19 or the restrictions on care at the time, but also included all the problems encountered and care required for people who continue to suffer and to die from a range of other illnesses even as the pandemic unfolded around them.
In this way, the principles and practices of palliative care have ongoing relevance across the board.
A key area frequently raised by the Sister Doctors was the burden of cancer treatments which were providing few benefits and causing severe financial hardship. The false hope that often accompanied these treatments could lead to patients having to travel significant distances, separating them from their families, while families who couldn’t afford the treatment could be left burdened with guilt.
The opportunity to offer palliative care for these people who were dying, and to consider and formulate this as a positive, and indeed the best option, was an important outcome of the course.

Echoing our work in implementing palliative care as part of best care or optimal care pathway – as currently enacted in the Care Plus study – this approach empowers the Sister Doctors and offers the patients and their families real hope for care, comfort and time with their community at the end of life.

Health & Medicine
The language of living and dying
While the online format has limitations – most particularly the difficulty engaging in person-to-person discussion – the energetic use of the Zoom chat function enabled significant interchange and, at times, parallel conversations.
The format also allowed 67 busy doctors from across India to come together with Australian colleagues to learn. These opportunities were highly valued.
As one participating Sister Doctor says: “During this COVID-19 pandemic era, I have seen a lot of patients dying without any help and in deep distress, also the family was in very (great) distress. So these meetings and discussions were very helpful. Thank you so much.”
Another participant wrote: “This course was a unique one ... though we are all far and wide, (we) came together to learn in our own places, presenting the cases with which we are dealing.”
The learnings were, of course, bilateral with the extraordinary experience of the participants shining through in all the ‘chat’ and discussion.

The Australian faculty were full of admiration for the creativity of palliative care delivery described by the Sister Doctors.
They spoke of palliative care which included not only care of the patient, and training family to help look after the person in their home, but also financial support for medications and assistance with facilitating employment of an otherwise out of work-family member who had ceased work in order to care.

Health & Medicine
The tech boosting world-class antimicrobial research
The opportunities to re-imagine what best care can be – including an expanded holistic view of palliative care – were richly shared across the Zoom spaces.
The partnership in palliative care continues beyond this training as further collaborative planning is underway. Importantly, the universal nature of problems faced by those with advanced illness means that further learning between and within countries like India and Australia is likely to be very rich.
Contributors to the collaboration also included Associate Professor Odette Spruijt, Founder and Chair of Australasian Palliative Link International; Dr David Brumley, Associate Professor Mark Boughey, Dr Anil Tandon and Professor Chitra Venkatesh.
The course was wonderfully supported by Professor Nathan Grills, and Dr Radhika Rohini, Mr Chiranjeevi Aruri and Rev Dr Father Mathew Abraham of CHAI.
The Sister Mary Glowrey Scholars program is supported by St Vincent’s Health, the Faculty of Medicine Dentistry and Health Sciences, Ormond College and Allan and Maria Myers.
Banner: Getty Images