
Health & Medicine
What’s the right COVID-19 risk to live with?

New epidemiological and economic modelling finds that elimination is better than a suppression strategy for COVID-19
Published 9 August 2021
It was the ‘big question’ of 2020 and remains so in 2021 – is an elimination strategy that tries to get rid of COVID-19 better than a suppression strategy that tries to control it?
Now, in August 2021 as the Delta strain of COVID-19 wreaks havoc both here in Australia and around the world, the question has become slightly different. It’s now “do we go really hard, really early when there is an outbreak?”.

And the answer now agreed by all, from the Prime Minister Scott Morrison down, is “yes”. Because once Delta gets its hooks into the community, it is so very hard to dislodge.
Back to 2020, here in Australia we had divergent views and actions across states and territories, and federally.
A consensus emerged on 24 July 2020 when the PM clearly stated the goal was zero community transmission, using an “aggressive suppression” strategy. This was really an elimination strategy, but was also cognisant that the virus would pop up again somewhere soon and require re-elimination.

Health & Medicine
What’s the right COVID-19 risk to live with?
The argument was that an elimination strategy would kill the economy and infringe civic freedoms by using lockdowns at a level of virus circulation that would not even lift an eyebrow in other countries.
The counter argument was that just sitting around and letting the virus get into the community, and then having to use lockdowns later to keep a lid on it when health services capacity was stretched, would turn out worse than going hard at the outset to eliminate it.
Our new research, published in JAMA Health Forum, aims to try and answer this question.
We used simulation modelling, calibrated to the data in Victoria and using the Victorian example (as the state came out of its second wave in August and September 2020).

But the lessons here can be broadly applied to other states or countries similar to Australia.
We used two models to answer the question.
Firstly, our agent-based model (ABM) that outputs daily infection rates went through thousands of runs to allow for uncertainty, like running a time machine over and over again.

Health & Medicine
Australia needs a more rational, evidence-based border policy
This ABM allowed us to simulate two elimination strategies where lockdowns were used early and hard to drive down numbers, and again when outbreaks occurred to re-eliminate the virus (there was a one per cent probability per day of the virus breaking out into Victoria due to a breach of quarantine).
And we compared it with tight and loose suppression strategies that attempted to keep virus levels at levels between one to five cases per million population per day (similar to South Korea in 2020) and five to 25 cases per million per day (similar to Europe in 2020), respectively.
The infection rates from the ABM were then put into a second model, called a proportional multistate life-table model, which estimates the health impacts in health adjusted life years and cost impacts – both health expenditure, and health expenditure plus Gross Domestic Product (GDP) costs.

That last bit is important. Because as we all know COVID-19 is more than just a health issue. We factored in – using government estimates – the GDP costs of lock downs.
What did we find?
Firstly, if you only consider the costs to the health system, elimination was the clear policy winner. This was unsurprising.

Politics & Society
Get ready for a shift in the COVID blame game
Any strategy that keeps the virus levels low will minimise SARS-CoV-2 morbidity and mortality, as well as health expenditure.
However – and this is where it starts to get more interesting – even when we allowed for the unintended consequences of lockdowns – like the worsening depression and anxiety and the reduction in road traffic injuries – they largely cancel each other out meaning elimination still won out.
However, if we include health and GDP costs, the situation becomes less clear.
Why? Because both strategies end up using lockdowns – the former early on when cases are low, and the latter when they are high.
The first figure shows that the two suppression strategies have less time spent in Stage 1a (very light restrictions, nearly like pre-COVID-19).
But all strategies see citizens subjected to considerable time in hard lockdown, with substantial overlap (shown by the black error bars) between the two elimination and two suppression strategies in the amount of time in lockdown.

If we then multiply these different times spent in varying levels of restrictions (five levels from Stage 1a to Stage 4) by Government estimates of the GDP cost of each level of restriction, we end up with the median (and 5th to 95th percentile) estimates of GDP loss for each strategy in Figure 1c (above).
And there is substantial overlap.
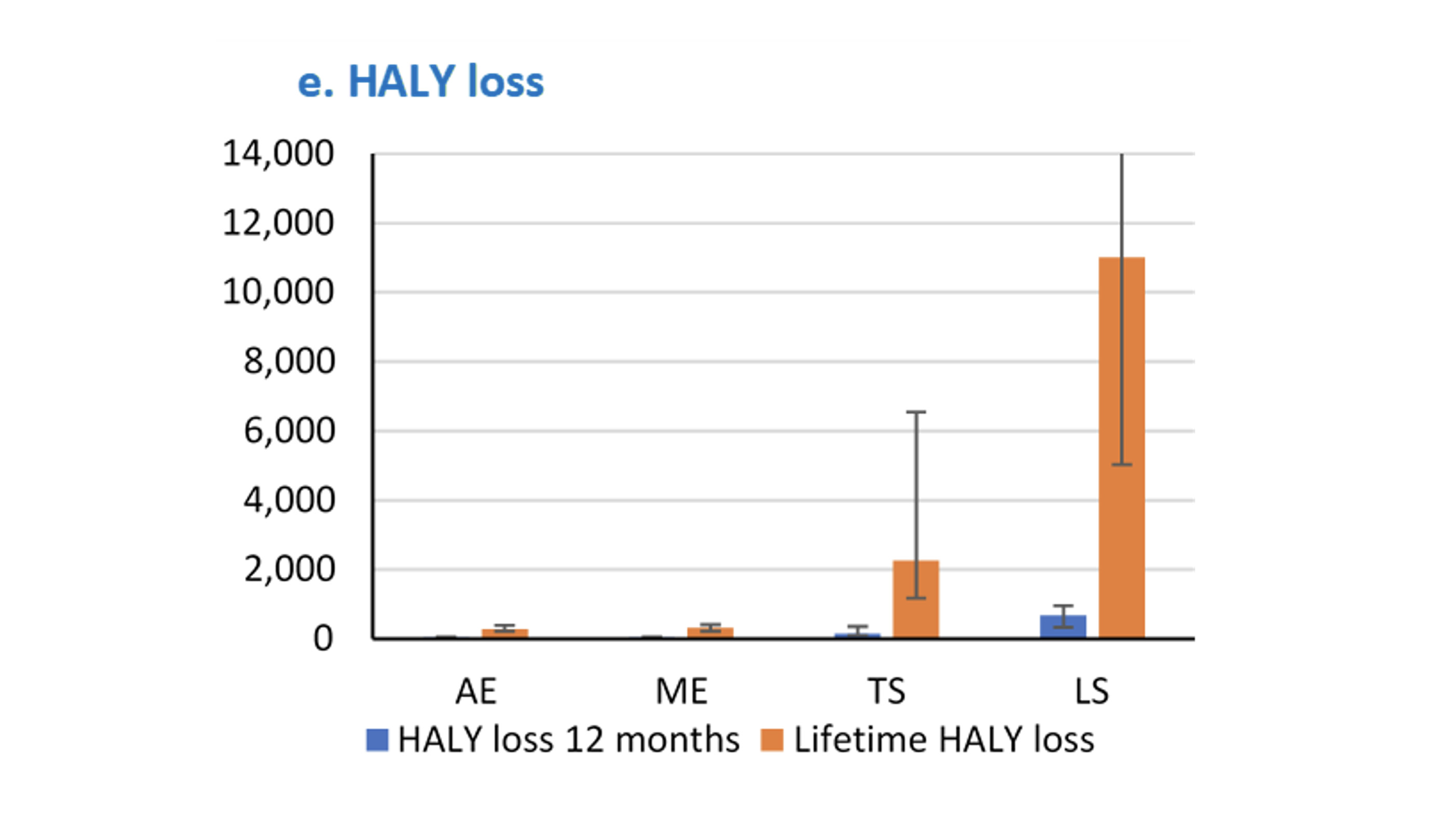
However, if we compare these four strategies within each iteration of the modelling (where the same values from uncertainty distributions of parameters like mask wearing efficacy are used – meaning the only residual variability is stochastic or chance), we do start to get a clear signal.
Namely, that for a usually accepted value of a health adjusted life year (or HALY), which is approximately $AU75,000 to $AU80,000 GDP per capita per HALY – in three quarters of the simulations one of the two elimination strategies (more often the ‘moderate elimination strategy’ as per the NSW approach in 2020) was preferred or ‘optimal’.
Put another way, on balance, an elimination strategy is preferred when considering health loss and costs – both health system expenditure and GDP loss.

Health & Medicine
How long till Sydney gets out of lockdown?
So that is what we make of elimination versus suppression in 2020. What can we learn for Delta in 2021?
As we all know, Delta is in another ballpark from the wild-type virus of 2020. And without doubt, for a country like Australia that took the elimination route – going very hard, very early, to stop any Delta outbreak – is the way to go now.
The best approach to Delta, if global eradication proves impossible, will tip from elimination toward suppression at high levels of vaccination coverage.
Exactly when it might do is far from clear – but more informed decision-making will be possible once there is over 80 per cent vaccine coverage, including children, in Australia. And this is what’s laid out (minus the children) in the Government’s plan.
Our team is continuing our work in this area. We are explicitly modelling how to open up as vaccine coverage increases.
You can explore this more at our regularly updated COVID-19 Pandemic Tradeoffs tool, and the Australian COVID-19 Modelling Initiative – a collation of modelling by a range of academic research groups that we are launching soon.
But the more information, data and modelling we have on COVID-19 – particularly the Delta strain – the more likely we are to be able to make informed decisions about the best strategy for Australia.
Banner: Getty Images