
Health & Medicine
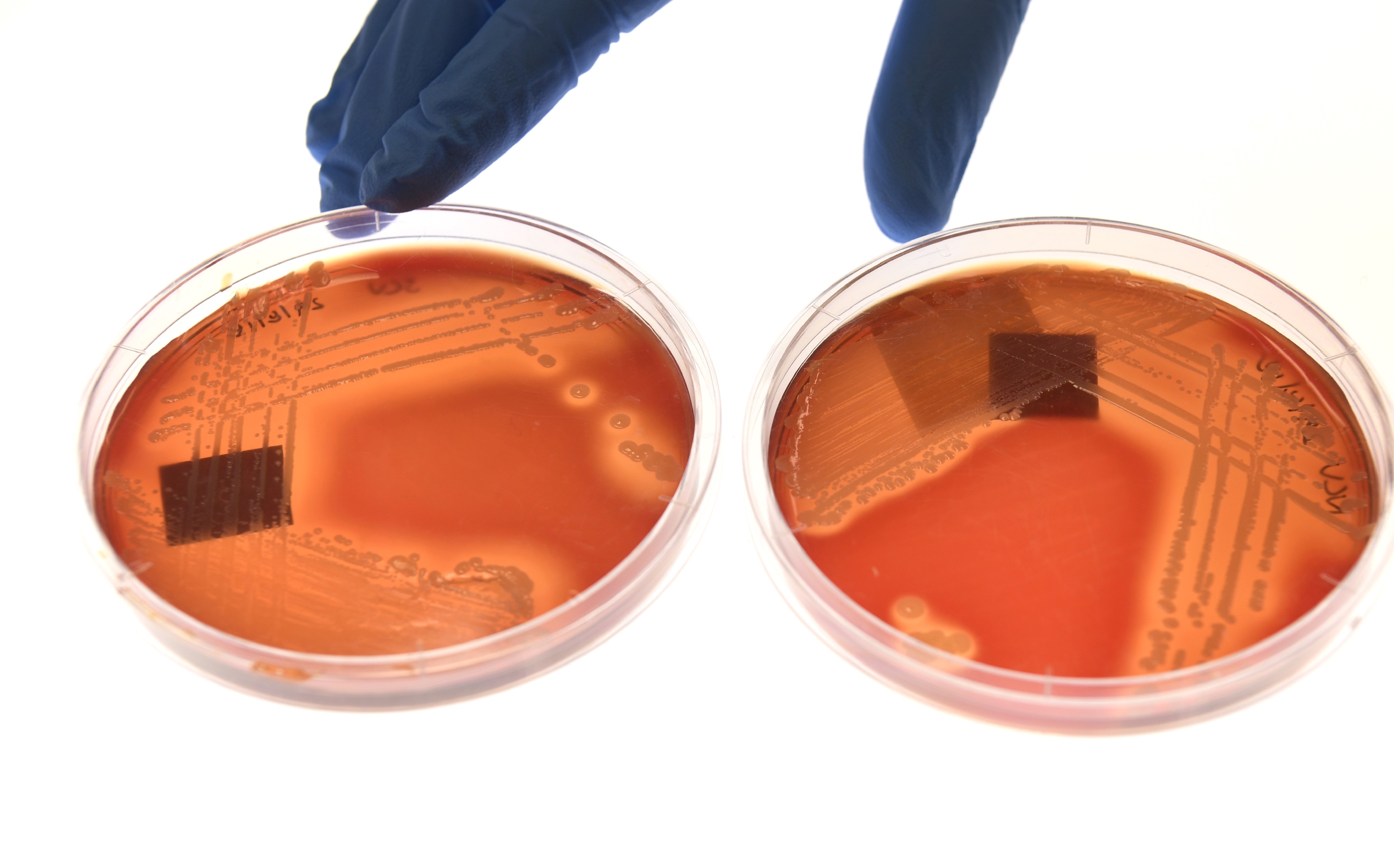
The rise of the latest drug resistant superbug

Managing the problem of antibiotic overuse and the treatment of sepsis concurrently can help to support better infection management
Published 15 November 2019
Every year, Antibiotic Awareness Week aims to raise awareness about the growing incidence of drug-resistant infections and the underlying phenomenon of antimicrobial resistance.
For many years now, healthcare workers have raised awareness about the problem of antibiotic overuse and now the message has started to get some traction.

To some extent, clinicians have succeeded in popularising the concept of antimicrobial stewardship – the practice of promoting judicious use, as well as reducing unnecessary or inappropriate use of antimicrobials.
There are two broad approaches to antimicrobial stewardship – the restrictive approach, where systems are put in place to monitor and rationalise antimicrobial prescribing, and the persuasive approach, where the hope is that education will improve decision-making.
But one of the key hurdles to implementing the restrictive approach has been a fear of sepsis.

Health & Medicine
The rise of the latest drug resistant superbug
Sepsis is the body’s overwhelming inflammatory response to infection. Many doctors fear missing sepsis, and this is not unjustified.
In a proportion of cases, sepsis can be seriously debilitating or even fatal. When severe sepsis isn’t treated in a timely manner, the consequences can be dire.
So, the problem of antimicrobial overuse has to be balanced with the problem of missed or delayed antimicrobial therapy.
It is, therefore, important for clinicians and healthcare workers to raise awareness about sepsis (and, within the healthcare system, appropriate therapy for sepsis), while talking about antimicrobial stewardship.
There’s a need to acknowledge prescribers’ fears about missing sepsis.
This represents the other side of the coin, where the focus of the awareness-raising activity is on promoting prompt and appropriate recognition of sepsis and commencement of therapy in hospitals. In the community we need people to recognise that sometimes we do require urgent care and shouldn’t delay seeking treatment.
Both approaches focus on the importance of patient safety.
Sepsis accounts for a large proportion of in-hospital mortality in Australia and around the world.

Health & Medicine
Stronger action to curb overuse of antibiotics
Sometimes, by the time that patients arrive in hospital with sepsis, it is already too late. Sometimes, as an ABC Four Corners episode showed earlier this year, even after the patient has arrived at the hospital, the signs and symptoms of sepsis are missed, and the patient deteriorates.
There are complex reasons for this.
It may be difficult to recognise the signs of sepsis, and there can be a lot of variation in how different clinicians and health services manage sepsis.
But there appears to be increasing awareness of sepsis in the community.
In 2016, an Australian survey showed that less than half of the people involved had heard of sepsis, and only a very small proportion recognised fever, rigors, rapid breathing, rapid heart rate and delirium as signs of sepsis.

Since then, a considerable amount of media coverage about sepsis seems to have built up a greater awareness about the condition in the community.
Importantly, sepsis care improvement and antimicrobial stewardship go hand-in-hand. Both are about enhancing the safety and quality of the treatment of infection.
When sepsis recognition and treatment are standardised, and this standardisation is embedded within the antimicrobial stewardship program, the de-escalation of therapy (the review and alteration of treatment in accordance with a patient’s microbiology results) can be properly managed.

Health & Medicine
The chemical warfare against bacterial superbugs
There is some concern that promoting faster initiation of therapy may have the unintended consequence of over-treating patients and this is a legitimate concern.
This is why embedding antimicrobial stewardship goals – like the promotion of appropriate antimicrobial use – within sepsis care initiatives is important.
Australian hospitals have made commendable progress in trialling system-wide initiatives to standardise and improve sepsis care – New South Wales, Victoria and Queensland have all trialled state-wide initiatives.
The Victorian sepsis pathway program focused on standardising and improving sepsis recognition and treatment across 11 health services in Victoria, and it generated encouraging results, including significant improvements in appropriate commencement of therapy in hospitals.

The program results included a 50 per cent decrease in mortality, a 34 per cent decrease in admissions to intensive care units (ICU), and improved time-to-treatment and quality of prescribing.
The results also showed a six-fold return on investment, with $A11.7 million saved through fewer ICU admissions and reduced length of stay.
So, a nationally consistent and coordinated approach can be beneficial, and there have now been calls for a nation-wide sepsis initiative.
We saw this with antimicrobial stewardship.

Health & Medicine
Improving how we manage sepsis
Clinicians and policymakers in Australia actively promoted the idea that there was a need for strategies to promote the careful use of antimicrobials within hospitals (to begin with).
The problem of rising rates of drug-resistant infections needed to be arrested and managed carefully, and one of the ways to do this was to rationalise antimicrobial use.
Australia developed educational resources, electronic workflow tools, clinical care standards, hospital accreditation criteria, a national action plan and a surveillance system to address this need.
We are still some way away from the goal of ensuring that all clinical settings – from tertiary hospitals to primary care clinics in the human health sector – have adequate support to promote the judicious use of antimicrobials.
But we have made some progress, and it’s worthwhile acknowledging how we got here.
Improving the quality of care and enhancing patient safety are the bedrock of both antimicrobial stewardship and sepsis care improvement, and, as clinical programs in Victoria have shown, developing both concurrently can support better infection management.
Banner: Getty Images